
Mclean/Shutterstock
After reading this article, you should be able to:
- Understand the importance of accurately triaging patients before offering a virtual consultation;
- Understand the importance of taking a patient-centred approach;
- Learn the skills required to provide an effective virtual consultation;
- Recognise the training and equipment required to provide effective virtual care.
A virtual or remote consultation is a scheduled appointment between a patient and healthcare professional for the purposes of clinical consultation, advice or treatment planning, conducted by phone or video[1]. Many pharmacists have experience with consulting remotely by phone, with these consultations facilitating services such as medication reviews, patient counselling and prescription verifications for patients.
The COVID-19 pandemic is responsible for driving a further shift away from face-to-face to remote or virtual consultations between patients and healthcare professionals[2–4].
With this trend likely to continue, pharmacists will need to develop skills and strategies to ensure virtual consultations are effective and person centred. This article aims to provide pharmacists with useful, practical tips and advice and considerations to ensure effective, person-centred virtual consultations.
1. Consider the benefits and risks of virtual consultations
Virtual consultations have many benefits when used across both primary and secondary care[5]. These benefits include:
- Avoiding or reducing unnecessary referrals;
- Reducing the need for patients to attend hospital, providing care closer to home;
- Improved patient experience and satisfaction (e.g. saving time and expense);
- Integrating primary and secondary care services, and increasing the use of a combined community service;
- Saving time by ensuring appropriate patients are seen either remotely or face-to-face;
- Meeting the demands of an increasing population;
- Reducing the environmental impact and number of journeys related to outpatient appointments in hospitals.
It should be noted that the evidence base for this change of practice is in its infancy and, although there have been no reports concerning the quality or safety of patient care to date, potential risks should be considered. These include poor patient management and missed or delayed diagnosis.
Pharmacists should report near-misses or incidents through their organisation’s usual channels, but may also find resources, such as the near-miss error log and near-miss improvement tools provided by the Royal Pharmaceutical Society[6]. As part of clinical governance requirements, pharmacy contractors need to report all patient safety incidents to the NHS[6]. One way to do this is via the Learn From Patient Safety Events (LFPSE) website. Some pharmacies may report incidents via their head office or superintendent pharmacist, who should report these in local risk management systems, as well as the LFPSE service[6].
2. Determine patient suitability and potential barriers
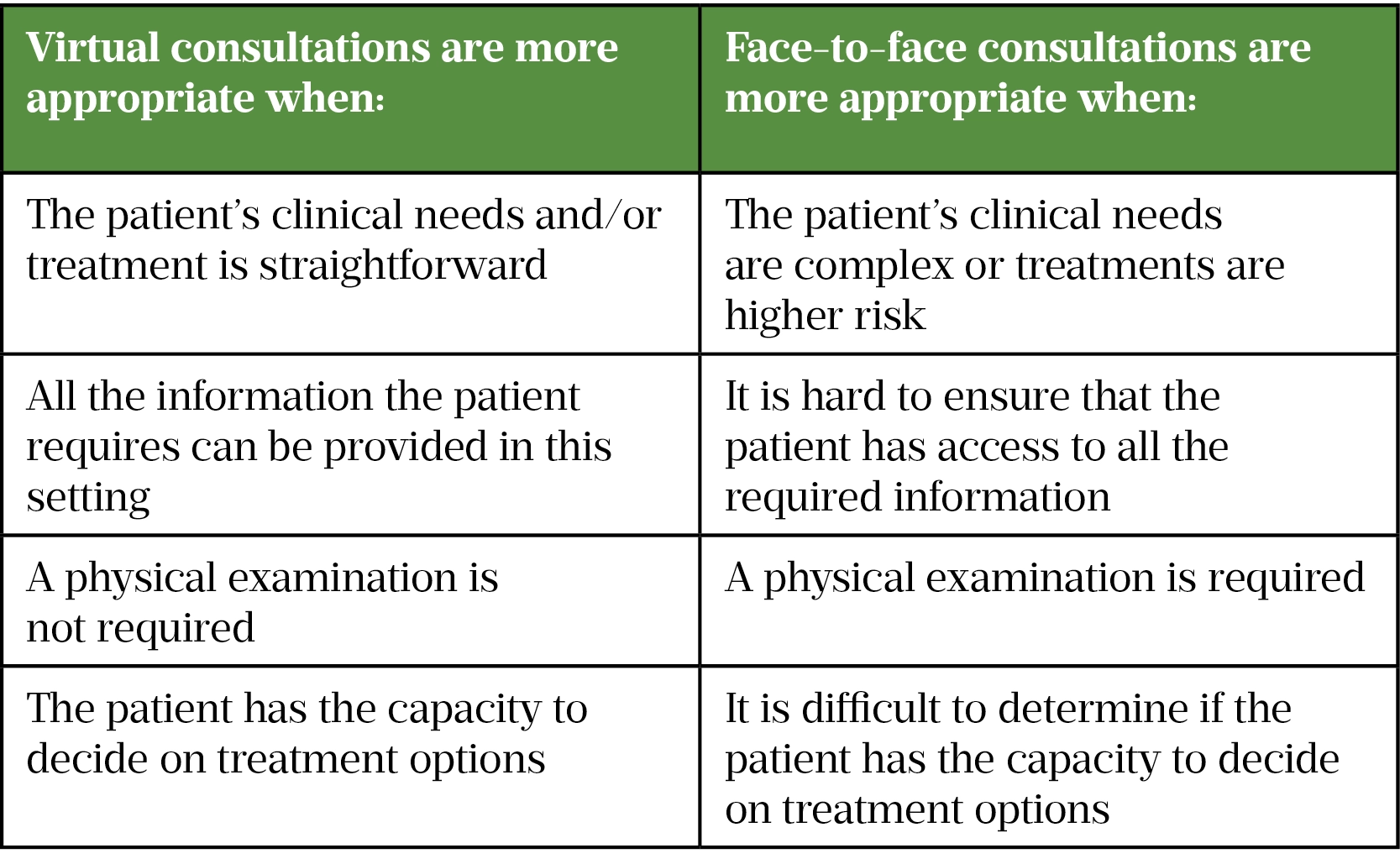
The choice of either a face-to-face or virtual consultation should be flexible and driven by the patient — for example, the patient may want a face-to-face appointment but may be happy with a virtual follow up. Table 1 outlines some important considerations when deciding between virtual and face-to-face consultations.
There may be additional barriers that prevent effective delivery of virtual appointments to specific patient groups, so healthcare professionals should look to accommodate the needs of each patient, as outlined below.
Access to technology
Around 16% of the UK population cannot undertake basic digital activities (e.g. connecting to wifi or turning on a device), with vulnerable and socially and economically disadvantaged groups most affected[8]. Patients who have insufficient access to, or are less competent with, technology will be better suited to face-to-face consultations. However, patients who face difficulties attending a face-to-face service (e.g. travel costs) may be more motivated to make a virtual consultation work.
At the beginning of a virtual consultation, check that the patient has privacy and access to a quiet space and that they are comfortable to continue the consultation.
Safeguarding and wellbeing
Medical records should be checked for any safeguarding concerns before the consultation.
If the patient is vulnerable or known to social care, the multidisciplinary team should discuss whether a face-to-face consultation would be more suitable. Any domestic issues, and the possibility of the patient being overheard in their personal environment, should be discussed with the patient when outlining their options.
Consider whether the virtual consultation will involve sharing emotionally distressing information. This may be easier when there is an established relationship with the patient. Most patients and clinicians prefer to share bad news through a face-to-face consultation[9]. However, the patient’s preference and circumstances are to be noted when determining the mode of delivery.
Language barriers, sensory impairment and disability
Pharmacists have access to interpretation and translation services for NHS patients. Clinical commissioning groups can provide access to interpreters to NHS patients registered under a GP within that location. Hospital trusts also provide their own translation services that have been approved by their trusts. Alternative access to translation sources in NHS England and South West can be found here[10].
Video consultations are still effective for patients who are hard of hearing if they can lip read. The UK charity SignHealth has developed some tips that can be used for communicating with deaf patients[11]. These include:
- Talking directly to the patient and not to any interpreters in the room;
- Using normal lip movements;
- Speaking at a normal speed.
When used efficiently, virtual platforms can be used to include patients who otherwise have difficulty accessing healthcare. However, for patients who lack digital literacy, simpler phone consultations or face-to-face consultations may be more suitable[12]. Some patients with learning disabilities and autism may also require face-to-face appointments because it is hard to ensure that the patient has all the required information.
Thinking about how gestures and facial expressions can be used to convey how serious something is to a patient can also be beneficial.
People living with frailty
As these patients are likely to be vulnerable and have more complex needs, they are usually best assessed in their home environment. If the patient is known, it may be easier to determine whether a virtual consultation would be suitable with a carer or family support.
Phone calls to the patient and/or their family or carer beforehand may help determine whether a virtual consultation is suitable. Virtual consultations may be better for individuals who find travelling to the pharmacy or hospital difficult.
Children
A virtual consultation may not be suitable for children as there may be a need for a physical examination, safeguarding concerns, or social/family interaction might be an important part of the consultation (this may still be possible with a virtual consultation, but needs consideration).
If a child does not have the capacity to consent (in line with Gillick competency), the usual position would be for someone with parental responsibility to communicate on their behalf.
Inclusion should be the core principle of virtual consultations and paediatric patients should receive the same level of access and consistent outcomes of care[13].
3. Consider setting up a triage system
Triage is required to prioritise patients according to urgency and type of treatment needed. Where possible, it is also important to acknowledge the patient’s preferences and could be established when the patient first contacts the healthcare provider. Benefits include better workflow organisation, fast-tracking patients who may need face-to-face or urgent care, and increasing opportunities for patient education and empowerment in managing acute problems[14].
Patients could make an enquiry online or by phone and their enquiries be filtered, with clinical queries sent to the most appropriate pharmacist, flagging urgent requests. The pharmacist can then review the query and respond through the most appropriate channel: an online message, video consultation, phone consultation or face-to-face consultation[15].
NHS England and Improvement has outlined how digital or phone total triage could work in practice. In a total triage system, all patients explain why they are making contact with the health service, so they can be triaged before making an appointment. Moorfields Eye Hospital, London, recently launched drop-in video consultations using the platform ‘Attend Anywhere’[15,16]. Between March and May 2020, 78.6% (260/331) of patients attending the video triage service in Moorfields A&E were able to avoid a hospital visit[16].
4. Have the right technology available and set up correctly
The room that will be used for the virtual consultation should be prepared in advance. It is recommended that a text and/or email should be sent to the patient, containing the details of the appointment and guidance on preparation for the virtual consultation (e.g. how to download any necessary software).
Having two screens will make it easier to access medical records and stay online with the patient at the same time. Using a headset may be useful, enabling better quality audio and cancelling out background noise. The patient’s phone number should be on hand, in case the video connection is not possible or fails, so that a phone consultation can be conducted instead.
In addition, for a phone consultation, both the patient and healthcare professional will need:
- A quiet place with good reception, free from disturbances;
- A working phone;
- To test the phone for clear reception before the scheduled call.
For a video consultation, both the patient and healthcare professional will need:
- A good internet connection;
- A quiet place with good reception, free from disturbances;
- A computer, tablet or smartphone with built-in camera and microphone;
- To test the equipment and software at the start of the day.
5. Reflect on the patient’s needs prior to and during the consultation
Inclusion should be the core principle of virtual consultations and patients should receive the same level of access and consistent outcomes of care as they would receive face to face[13]. Barts Health NHS Trust has developed a guide for clinicians on video consultations that outlines when a virtual consultation may be suitable for the patient and how to prepare for the video consultation[17]. When the patient/healthcare professional relationship is new, the PATIENTS mnemonic (see Box) can be useful in ensuring the consultation focuses on the patient’s needs and on building rapport[18].
Box: The PATIENTS mnemonic for virtual consultations
Personal — use the patient’s name and show interest in them.
Ask — how the patient is, what they would like to get from this consultation, if they have any worries or if there is anything they would like you to know.
Timings — a one-hour appointment window is reasonable. Confirm that it is a good time to speak. Acknowledge if you have called early or kept the patient waiting.
Important — find out what is most important and what matters to the patient.
Empathy — show empathy by giving the patient time and space to feel, think and speak.
No acronyms — use clear, straightforward language and avoid medical terminology; however, avoid ‘dumbing down’ or patronising the patient.
Tune in — listen to the patient and do not rely on an agenda. Ensure the patient is heard and understood.
Support — work with the patient to explore what support they have or need, what would help them and how you can provide support. Patients often have the best and most suitable solutions.
Source: Adapted from ‘How can you make the most of your virtual consultation’, South East London Cancer Alliance [18]
At the beginning of the consultation, ask the patient if the appointment time is still a good time to talk and if they have a quiet or private space. If this is not the case, the consultation should be rearranged.
The pharmacist should introduce themselves, their role and any colleagues with them, as well as the purpose of the consultation.
6. Develop the right communication skills
During a video consultation, enhanced non-verbal communication is advantageous. For example, establish eye contact by looking at the camera and not at the eyes of the patient, so that they feel acknowledged.
Be sure to remember to obtain consent, introduce any colleagues present in the room, and inform the patient when taking notes (as the patient may feel disregarded when eye contact is lost)[18].
The CONSULT (consider, organise, necessary, start, undertake, listen, terminate) guide, previously outlined in ‘Remote consultations: how pharmacy teams can practise them successfully’ can help clarify whether a remote consultation is appropriate and help pharmacists and the pharmacy team understand how to approach the process[19].
For other guides and tools, see ‘Useful resources’.
7. Learn and follow the rules around data protection, confidentiality and consent
A virtual consultation should offer the patient security and confidentiality, just as in a face-to-face consultation. Where this is not possible, a face-to-face consultation should be considered.
Document the details of the consultation clearly, including the time and date, being specific about how information was obtained. The consultation should not be recorded (video or audio) unless there is a justifiable reason that has been discussed with the patient, and informed consent has been obtained and accurately documented. If recording, indicate to the patient when recording has started and has been stopped, and store the recording securely in the patient’s clinical record[20].
Only platforms provided by the NHS or other approved regulators should be used to share patient data[14]. Follow your organisation’s policy on the secure management of patient data, in accordance with the Data Protection Act 2018 and GDPR[20]. The Information Commissioner’s Office should be notified of any data breaches immediately and within 72 hours. Data subjects must also be notified if the breach could have an adverse impact[20].
At the start of the consultation, consent should be requested. The pharmacist should be mindful that the patient can withdraw their consent at any time.
8. Ensure you check patient understanding and safety-net appropriately
It is important to use clear language, check that the patient understands what has been discussed and that appropriate safety-netting has been covered[21]. If available, the chat function on video calls or text should be used to send links to advice or patient information leaflets that the patient can access later. Pharmacists should inform patients of any warning signs and/or worsening symptoms. Where more urgent medical attention may be required, actively signpost patients to support. Patients should be advised on where to go according to the severity of their symptoms (e.g. A&E, NHS 111, GP or pharmacy) and who to contact if a service is unavailable[21].
The pharmacist should explain what the patient should expect after the consultation and how to seek further advice if the expected outcome is not reached. Pharmacists should also consider setting up a scheduled ‘check in’ with the patient to monitor the patient virtually. For example, the patient could be sent a brief questionnaire about their symptoms[21].
9. Know when to seek support and advice
Shifting from normal practice to remote consultations can be difficult, particularly during the pandemic. One of the challenges highlighted by the Health Foundation’s Scaling Up programme at Barts Health Trust was ensuring continuity of care during remote consultations[22]. Having a positive, pre-existing relationship between the patient and clinician affected the quality and flow of remote consultations[22]. Newham Hospital, London, used a hybrid approach of face-to-face initial appointments and follow-up remote clinics[22].
Having empathy and person-centred communication was also described as a challenge in remote consultations[22]. Making eye contact and understanding verbal and non-verbal cues may be difficult to convey or pick up on in remote clinics, especially phone consultations. Pharmacists should practise self-care so they can effectively look after their patients. Support and advice should be sought from colleagues when required, and sharing experiences in practice with others can help develop and adapt the service — for example, through the discussion of clinical cases or developing a process for peer-to-peer support for dilemmas[12]. Self-audits of consultations are encouraged, and patient feedback should be sought and reviewed (e.g. through short online surveys)[12].
Useful resources
- The Royal College of Psychiatrists’ 6 Cs shows how to deliver an effective virtual consultation;
- FutureLearn runs courses on how to conduct virtual consultations, including how to triage patients, history taking, safe patient management and taking essential observations;
- The Centre for Pharmacy Postgraduate Education module on virtual consultation skills.
- 1Clarke G, Pariza P, Wolters A. How are total triage and remote consultation changing the use of emergency care? The Health Foundation. 2022.https://www.health.org.uk/news-and-comment/charts-and-infographics/how-are-total-triage-and-remote-consultation-changing-the-us (accessed Mar 2022).
- 2Gilbert AW, Billany JCT, Adam R, et al. Rapid implementation of virtual clinics due to COVID-19: report and early evaluation of a quality improvement initiative. BMJ Open Qual. 2020;9:e000985. doi:10.1136/bmjoq-2020-000985
- 3Greenhalgh T, Vijayaraghavan S, Wherton J, et al. Virtual online consultations: advantages and limitations (VOCAL) study. BMJ Open. 2016;6:e009388. doi:10.1136/bmjopen-2015-009388
- 4RCGP survey provides snapshot of how GP care is accessed in latest stages of pandemic. Royal College of General Practitioners. 2020.https://rcgp-website-delivery-uk.azurewebsites.net/about-us/news/2020/july/rcgp-survey-provides-snapshot-of-how-gp-care-is-accessed-in-latest-stages-of-pandemic.aspx (accessed Mar 2022).
- 5What are the aims, benefits and risks of non face-to-face clinics? UCL Partners. 2022.https://uclpartners.com/non-face-to-face-clinics-resource/what-are-the-aims-and-benefits-nf2f-clinics/ (accessed Mar 2022).
- 6Patient safety incident reporting. Pharmaceutical Services Negotiating Committee. 2022.https://psnc.org.uk/contract-it/essential-service-clinical-governance/patient-safety-incident-reporting/ (accessed Mar 2022).
- 7Remote consultations flowchart. General Medical Council. 2022.https://www.gmc-uk.org/ethical-guidance/learning-materials/remote-consultations-flowchart (accessed Mar 2022).
- 8Lloyds Bank UK Consumer Digital Index 2020. Lloyds Bank. 2020.https://www.lloydsbank.com/assets/media/pdfs/banking_with_us/whats-happening/lb- consumer-digital-index-2020-report.pdf (accessed Mar 2022).
- 9Poovamnilkunnathil A, Nabhani-Gebara S, Dalby M. 1625P The virtual clinic: An insight into the patient and clinician experience in cancer during COVID-19. Annals of Oncology. 2021;32:S1154–5. doi:10.1016/j.annonc.2021.08.1618
- 10West N. Interpretation and Translation Services. NHS England and NHS Improvement South West. 2022.https://www.england.nhs.uk/south/info-professional/pharm-info/language-and-intepretation/ (accessed Mar 2022).
- 1112 tips for communicating with deaf patients. SignHealth. 2022.https://signhealth.org.uk/resources/learn-about-deafness/tips-for-communicating-with-deaf-patients/ (accessed Mar 2022).
- 12London networks good practice guidance to determine suitability of remote consultation. NHS England and NHS Improvement. 2020.https://selondonccg.nhs.uk/wp-content/uploads/2020/08/Paper-1b.-Remote-consultation-good-practice-guidance-Draft-v-1.0-for-CAG_.pptx (accessed Mar 2022).
- 13Unlocking the digital front door. National Voices. 2021.https://www.nationalvoices.org.uk/sites/default/files/public/publications/unlocking_the_digital_front_door_-_keys_to_inclusive_healthcare_report.pdf (accessed Mar 2022).
- 14Macwilliam J, Hennessey I, Cleary G. Telemedicine: improving clinical care and medical education in paediatrics. Paediatrics and Child Health. 2021;31:388–96. doi:10.1016/j.paed.2021.07.004
- 15Digital first: moving to online triage and consultations. NHS England and NHS Improvement. 2020.https://www.youtube.com/watch?v=sczwFG6fxZM (accessed Mar 2022).
- 16Remote consultations to reduce hospital and primary care visits for urgent eye care services. NHSX. 2021.https://www.nhsx.nhs.uk/key-tools-and-info/digital-playbooks/eye-care-digital-playbook/remote-consultations-to-reduce-hospital-and-primary-care-visits-for-urgent-eye-care-services/ (accessed Mar 2022).
- 17Greasley A. Video consultations. Barts Health NHS Trust. 2021.https://www.bartshealth.nhs.uk/video-consultations (accessed Mar 2022).
- 18How can you make the most of your virtual consultation? South East London Cancer Alliance. 2021.https://www.selca.nhs.uk/news/how-can-you-make-most-your-virtual-consultation (accessed Mar 2022).
- 19Remote consultations: how pharmacy teams can practise them successfully. Pharmaceutical Journal. 2020. doi:10.1211/pj.2020.20208102
- 20Data protection, remote working and COVID-19. LawWorks. 2022.https://www.lawworks.org.uk/solicitors-and-volunteers/resources/data-protection-remote-working-and-covid-19 (accessed Mar 2022).
- 21Principles for supporting high quality consultations by video in general practice during COVID-19. NHS England and NHS Improvement. 2020.https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/C0479-principles-of-safe-video-consulting-in-general-practice-updated-29-may.pdf (accessed Mar 2022).
- 22Horton T, Jones B. Three key quality considerations for remote consultations. The Health Foundation. 2020.https://www.health.org.uk/news-and-comment/blogs/three-key-quality-considerations-for-remote-consultations (accessed Mar 2022).


