Key points
- Simulation-based training (SBT) is an innovative training technique that has been increasingly used in healthcare over the past few decades.
- A variety of simulation technologies are available to support skill development, including patient simulations, computer-based simulations and virtual reality simulations.
- SBT can be used to provide a safe environment for pharmacists to develop their professional skills.
- SBT can help develop technical and non-technical skills, including communication, team working, decision making and task prioritisation.
- SBT can assist in individual or multiprofessional team training, with the potential to enhance team performance and patient safety.
Introduction
The role of the pharmacist in UK hospital settings has changed significantly over the past 15 years, from a medication-centred to a more patient-centred role. Examples of this evolution and development include enhanced roles in medicines reconciliation, attendance on ward rounds, leading outpatient clinics and development of clinical speciality and prescribing roles[1]
.
With the evolving role of pharmacists and the growing complexity of healthcare, there is a need for interventions and innovations to enhance both individual task and team performance. Simulation-based training (SBT) is an educational platform with potential in this area. This article outlines its applications in pharmacy and how it can support the skill acquisition and development of pharmacists.
Sources and selection criteria
Cumulative Index to Nursing and Allied Health Literature and PubMed (National Library of Medicine) were used to review relevant publications for this article. A general internet search was also carried out to identify relevant non-indexed content. Searches were limited to English language articles with no restrictions on the age of the article. Search terms included pharmacist (OR pharmacy) and simulation (OR simulation-based training). Similar terms were used to find relevant articles for the use of SBT in healthcare, including nursing and medicine. Each reference was reviewed for relevance and quality by the authors for inclusion in this article.
Simulation-based training
Simulation has been defined as “a technique, not a technology, to replace or amplify real experiences with guided experiences, often immersive in nature, that evoke or replicate substantial aspects of the real world in a fully interactive manner”[2]
. Here, a simulation technique is used, utilising a device, such as a ‘standardised’ patient or mannequin, to teach healthcare professionals a relevant skill or process, helping them improve competence and ensure a safe level of care[3]
.
SBT allows learners the opportunity for deliberate practice in a safe environment where they can respond to high-risk situations, make mistakes and learn from any errors[3],[4]
,[5]
. Using simulation avoids inconveniencing patients by repeatedly involving them in training scenarios, or putting them at risk from error[6],[7],[8]
.
Situations that could be stressful, infrequent or dangerous can be replicated through SBT. The controlled scenario allows for exposure to specific learning outcomes that can be standardised across all participants, allowing a platform for both formative and summative assessment as part of further study or competency programmes. It can also be used to allow controlled exposure to clinical scenarios of increasing complexity, in order to support individuals in developing more advanced clinical skills. SBT can also provide a unique opportunity for teams to work together and develop the non-technical skills required for the successful execution of tasks in clinical environments.
Educational benefits
Didactic teaching is insufficient for dealing with crises or rare clinical conditions[9]
, or for team-based training or activities that require retention of knowledge and skills beyond a year[10]
. Lectures and tutorials have traditionally been the core methods used to teach pharmacy students and pharmacists[11]
, although lectures can limit development of skills required for clinical practice[12]
.
By contrast, SBT can offer a rich, learner-centred educational platform and provide meaningful experiences where participants can reflect on identified knowledge gaps[13],[14]
.Evidence demonstrates that profound educational experiences are emotionally charged and challenging, with optimally designed SBT stimulating meaningful reflection to influence behaviour.[13],[14]
For any team-based SBT, a community of practice can be developed, which can have benefits that reach beyond the learning experience[15]
. SBT can be used to enhance team performance[16],[17]
, supporting patient safety outcomes through increased collaboration, reduction of error, and development of teamwork and communication skills[3],[18],[19]
.
SBT in healthcare involves adult learners and independent practitioners. Adult learners are often intrinsically, rather than externally, motivated[20]
; therefore, it is important that the learning outcome is practical, immediately usable and relevant. It has been proposed that adults learn best when they participate, are engaged, and experience teaching in a cognitive and emotional way[21]
. Experiential learning is a process where experience is transformed into learning[22]
. This is reflected in a four-stage learning cycle of learning (see Figure 1), familiar to pharmacists through continuing professional development, which includes experience, reflection and experimentation — key components of SBT[22]
.
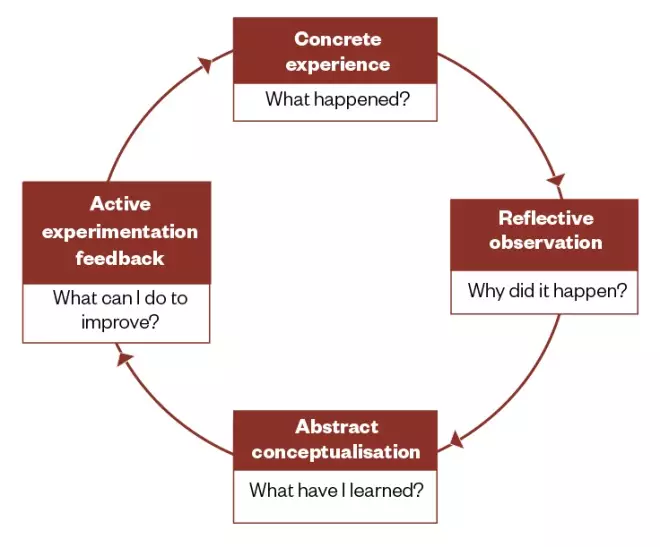
Figure 1: Kolb’s experiential learning cycle
Simulation-based training can provide a tangible experience and reflective observation, allowing learners to conceptualise new mental models that can be actively tested.
The cycle begins with an experience (the SBT) that offers the chance for learners to identify knowledge gaps and reflect on their performance. Here, SBT is catalysing the learning process by providing an opportunity for observation and reflection. Reflection can be facilitated by educators who debrief on the simulation[14]
. This then allows for abstract conceptualisation, shaping the learner’s mental model through analogical reasoning, allowing consideration of outside information from the educator to make sense of the experience[14]
. This can inform future behaviour and decisions and be actively tested in practice, allowing the cycle to begin again. Feedback is a critical process of SBT and, as an educational tool, can reduce the gap between perceived and actual performance of learners, supporting reflection on performance and guiding progression through the learning cycle[23]
.
Application of SBT
SBT has been used extensively in the aviation and aeronautical space industries, as well as in the military, chemical and nuclear power sectors where its efficacy and safety have been demonstrated[24]
. In healthcare education, where learning experiences can be limited, where it is unethical to practice on patients, and/or where it could compromise patient safety, there is potential for the application of SBT. It is often used to develop and assess technical and clinical skills for healthcare professionals[3],[25]
(e.g. blood pressure measurement, cannulation or catheter insertion). SBT is also used to develop and assess non-technical skills, defined as cognitive, social and personal resource skills[26]
(e.g. communication, teamwork, task prioritisation and decision making).
Crew resource training
Several publications have raised awareness around potential sources of error and the need to reduce avoidable harm in healthcare[27],[28]
.’ Around 20 years ago, the need for crew resource management training in healthcare (initially called ‘cockpit resource management training’), similar to the aviation industry, was described to develop the non-technical skills of staff and improve patient safety[27]
. Crew resource management training provides traditional didactic teaching on a subject, with hands-on experiential learning for the whole team through simulation, improving teamwork and non-technical skills[29]
.
Non-technical skill development
In addition to developing technical proficiency, SBT has also been used to develop and enhance team performance and non-technical skills and behaviours for specific situations[16]
. These are the cognitive, social and personal resource skills that complement technical skills, supporting safety and task performance[26],[30]
. Cognitive skills include decision making, planning and situational awareness, while social skills include teamwork and communication[30]
. These skills are increasingly recognised as critical in optimising prescribing outcomes[31]
, and a recent review reported that moderate-to-high quality evidence suggests team training can positively impact healthcare team processes and patient outcomes. In addition, bundled team training interventions and implementation strategies that embed effective teamwork as a foundation for other improvement efforts may offer the greatest impact on patient outcomes[32]
.
The simulation session
Simulation sessions should be carefully designed to ensure they are aligned with relevant curricula, performance standards and learning outcomes. Educators should consider the purpose of the SBT and whether students will be prepared for the session to simulate dealing with the unknown, or if they will be provided with background information in the form of videos or lectures in advance. The introduction to learning material ahead of the session utilises a flipped classroom approach that can cognitively prepare learners for the simulation, promote interest in learning and allow them to build on existing knowledge, and focus on the SBT learning experiences[33],[34]
. However, this approach requires students who are self-motivated; when students do not engage with the pre-learning activities, the SBT may be ineffective[35],[36]
.
Planning of any simulation session should include the type of simulation and scenario design, including relevant materials, patient training, transcripts and potential responses to treatment. Any planning should also consider the facilitation and briefing on the scenario so that participants are clear on the objectives before commencing the simulation.
Simulations can vary in their technical complexity and psychological, environmental and technological fidelity (level of realism). The level of fidelity required should be considered when designing SBT, with the learning outcomes influencing the types of simulation used and resources required.
Types of simulation used in healthcare
Each simulation technique has the potential to provide different learning and development opportunities for pharmacists, depending on the intended learning outcome and required fidelity (see Table 1).
| Simulation intent | Potential applications | Simulation equipment | Environmental placement | Psychological fidelity |
|---|---|---|---|---|
| Individual skill acquisition | Cannula insertion, blood pressure monitoring, prescription review | Part-task trainer, such as an artificial arm or medication chart | Classroom based | Low |
| Individual skill acquisition with communication | History taking and assessment, patient counselling, communication skills, medicines information scenario, dealing with error, performance assessment | Part-task trainer with standardised patient | Classroom, clinical skills laboratory | Low to medium |
| Multiprofessional team resource management in simulated area | Management of specific clinical conditions, response to emergency situations/crises, preparation for being on-call. Developing non-technical skills, such as team communication | High-technology patient simulator, standardised patient | Simulation suite | Medium to high |
| Multiprofessional team resource management. Full environment simulation | High-impact multiprofessional team simulation for management of clinical scenarios. System testing and capture of error-provoking factors | High-technology patient simulator, standardised patient | Clinical area | High |
Technological fidelity relates to how the simulation duplicates the appearance of the system or patient, whereas environmental fidelity is concerned with environmental cues and stimuli of the task environment. However, psychological fidelity concerns the degree to which the trainee or student perceives the simulation to be a believable task replacement. This is considered the most essential requirement to suspend disbelief, requiring high task fidelity and functional fidelity so that the SBT both resembles and responds like real life.
SBT can vary from low- to high-fidelity scenarios that are delivered in a simulated environment, or in situ in the clinical environment using patient simulations. The purpose of the SBT and intended learning outcomes will influence construction of the SBT event, including resource considerations such as the type of patient simulation.
Training can include patient simulations, computer-based learning simulations and virtual reality (VR) patients[37]
. Patient simulations broadly include two large groups which can include sophisticated mannequins and various part-task trainers[38]
, and standardised patients consisting of paid actors, faculty members or students[38],[39],[40]
.
Various types of mannequins are available in healthcare simulation, although they all share the same characteristic of using technology to enhance learning. Modern SBT in healthcare can be traced to the use of the Resusci Anne mannequin for effective mouth-to-mouth ventilation and chest compressions in the 1960s; mannequins have since been developed to simulate various diseases, allowing learners to develop the skills to manage these conditions[38],[41]
.
With advancing computer software and technologies, more complex high-fidelity mannequins that can talk, breathe and have realistic heart and lung sounds are available in healthcare education. They can also be programmed with greater sophistication and learner interactions that replicate physiological parameters and responses to procedures and treatment, including medication administration with appropriate physiological responses. Examples include the SimMan® 3G (Laerdal Medical; see Figure 2), Human Patient Simulator (METI) and Emergency Care Simulator (METI) that can be programmed for a wide range of scenarios.
Part-task trainers may also be used that allow learners to develop specific skills in isolation and provide low-to-medium fidelity experiences[42]
. Examples include practising blood pressure measurement on an artificial arm, screening a prescription for errors and accuracy, or standardising documentation in patient notes.
Other technologies used in SBT can include computer-based learning programmes and VR simulators. Here, the learner follows a programmed sequence, interacting with the environment through the computer or VR headset[43],[44]
. Evidence shows that use of this technology supports clinical reasoning and communication skills, and increases healthcare professionals’ knowledge[45],[46]
. Simulated electronic patient records have also been used to assess and support development of the accuracy of documentation in medical notes[47]
.
‘Standardised’ patients are where a lay person, actor, faculty member or student peer are used to simulate the scenario or clinical condition[40],[48],[49]
. They were introduced in the 1960s to assist in the training and assessment of communication, physical assessment and examination, professionalism and clinical skills[38],[41]
, and are commonly used in the training and assessment of pharmacists in patient counselling or throughout objective structured clinical examinations[40],[48],[49]
. The use of standardised patients allows learners the opportunity to practice clinical skills as necessary, with provision of targeted facilitator feedback in a safe and controlled environment. When used in assessments, the standardisation can ensure fairness and valid comparisons in performance[40]
. In addition, standardised patients offer the advantage of removing risk to patients[7],[40],[50]
and can increase the fidelity of the experience in comparison to a mannequin. However, use of standardised patients can be associated with significant costs for payment of actors or faculty[48]
, while the time required to prepare scenarios and train the individual can be substantial[40]
.

Figure 2: Mannequin-based simulation
An example of SimMan® 3G (Laerdal Medical) in a simulation training suite used to optimise simulation training and support technical and nontechnical skill development.
Full environment simulation involves high-fidelity mannequins and standardised patients, an authentic clinical environment and healthcare professionals with relevant equipment. This environment could be a simulation suite or simulated exercise that is delivered in situ with authentic materials and equipment, increasing the level of fidelity and providing a highly immersive experience (see Figure 3).
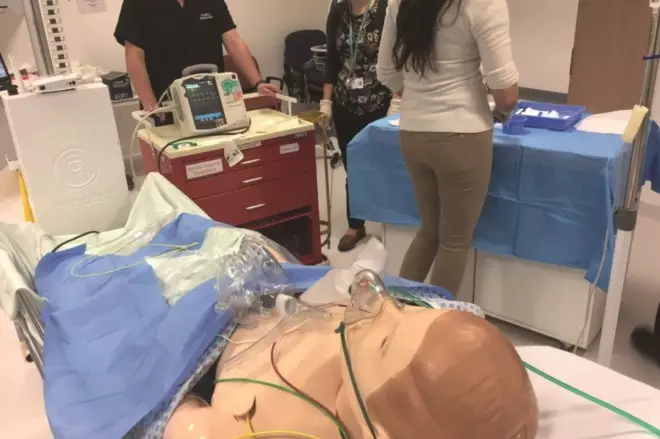
Figure 3: Multiprofessional simulation team
A simulated clinical scenario using SimMan® 3G (Laerdal Medical) for multiprofessional team training, facilitated by a simulation tutor.
Debriefing
Participant debriefing is a critical component of simulation for effective learning and should be planned as part of the learning session[20]
. The concept originates from the military sector where participants would describe what happened on a mission, with analysis used to develop strategy for future missions[20]
. In healthcare, debriefing is used to promote improved performance in similar future situations[51]
.
Debriefing allows the opportunity to explore the skills, knowledge and attitudes that influenced a participant’s actions[52]
, and is critical to presenting the outcomes of the simulation and evaluating perceptions of participants’ own performance[9]
. The debriefing process facilitates reflection on the simulated scenario through active participation in conversation between the educator and learner or participant[7],[53]
, typically immediately following the simulation[54]
. The benefits of debriefing in supporting development of interprofessional teams has been described[55]
and similar positive outcomes would be expected with pharmacist involvement.
In healthcare, this can often involve participants watching a video recording of the simulated event, with a facilitator guiding participants to reflect on their performance. This technique has been demonstrated to encourage reflection, identify performance gaps and improve future performance[56]
.
Debriefing is considered one of the most challenging aspects of SBT[54]
and requires skilled individuals to both assess and facilitate the process. These facilitators should be trained in the delivery of feedback to ensure successful outcomes are achieved[52]
. To support the debriefing process, various frameworks are available to educators to support practice[53],[57]
. Debriefing requires a psychologically safe environment to explore meaning behind a learner’s actions. Facilitators share their observations and insights with the learner, which are then explored. This is a good judgement approach, valuing both learner and facilitator perspectives to illuminate and understand learner behaviour[51]
.
This process can explore both positive and negative aspects of the simulation performance[53],[57]
. Here, as well as exploring any reasons for failure by focusing on ‘work as done’ (a ‘safety 1’ approach), there is opportunity for learners to reflect on and learn from what went well. The reasons and behaviours for performing ‘work as imagined’ (a ‘safety 2’ approach) is increasingly advocated for safety management to understand good performance in different contexts[58]
. There is growing recognition for this approach in healthcare and SBT[59],[60]
, where individuals and teams can learn from success or exceptional performance, as well as failure[16],[53],[58],[61]
,[62]
.
SBT in healthcare education
Increasing use of SBT in healthcare education has been observed in recent years[52]
, with the main aim of optimising patient care and safety, while allowing standardisation of training and assessment, and practicing skills in a controlled environment[2]
.
A wide range of simulation technologies are commonly used in healthcare education to support knowledge acquisition, critical thinking and clinical skills, such as medicines administration and management of emergency situations[63],[64]
, while also improving the confidence or trainees[65]
. SBT is widely used in both undergraduate and postgraduate medical curricula in the UK to enhance performance[37]
. It is becoming accepted as the industry standard for the education and training of nurses and doctors[66]
, with the effectiveness of SBT as a replacement for nursing hours demonstrated[67]
.
However, the use of SBT has not evolved to the same level within pharmacy education[7],[48]
and high-fidelity SBT is still in its relative infancy in the UK[68],[69]
. The remaining sections below describe the potential applications of SBT in developing the skills and enhancing the performance of pharmacists.
SBT for pharmacists
Potential applications of SBT to support development of pharmacists’ technical, cognitive and non-technical skills are outlined in Table 2.
| Potential simulation scenario | Potential learning outcomes | Suggested resources |
|---|---|---|
| Medication history taking |
|
|
| Interprofessional communication |
|
|
| Medication review/prescribing error resolution |
|
|
| High-risk or routine clinical scenario |
|
|
| Medicines information (including on-call) |
|
|
| Medication safety |
|
|
The literature supporting the use of high-fidelity SBT for pharmacy in the UK is limited, with the majority of evidence emerging from the United States[68],[69],[70]
. This could be influenced by the perceived traditional supply role of a pharmacist having less direct patient contact compared with nurses and doctors. The role of pharmacists in the UK has evolved considerably in recent years towards a greater patient-centred role and, therefore, demands enhanced clinical skills[1]
. However, as undergraduate pharmacy is funded differently to medicine and nursing programmes, the opportunities for clinical placements for pharmacy students can be limited[71]
. Such limited exposure to clinical practice can create a mismatch between student expectations and the reality of clinical practice, with pharmacists requiring skills of a different order than can currently be achieved at registration[72]
. SBT could be used to both supplement these experiences and support development of clinical skills as part of any ongoing postgraduate training, helping to better prepare and support pharmacists in clinical practice.
High-fidelity SBT can provide a safe and controlled learning environment for pharmacists to apply their knowledge and develop their professional skills[73],[74]
. SBT is well received by pharmacy students and has been shown to improve confidence[75]
, enhance learning and improve test scores in the management of clinical conditions, medication administration or drug calculations[42],[68],[76],[77]
. Recently, the use of a computer-based simulation was reported to support self-directed learning and develop decision-making skills of pharmacy students in an oncology pharmacotherapeutics programme[78]
. Elsewhere, SBT has been shown to enhance pharmacy student performance in monitoring drug treatment[79]
and clinical skills such as blood pressure measurement[75]
. In emergency situations, SBT has been reported to enhance problem-solving skills[74]
and understanding of the role of pharmacists in managing these conditions[8],[77]
, although benefits also extend to routine clinical scenarios[9]
.
SBT has also been shown to enhance pharmacist communication, critical thinking and team-working skills[6],[68],[76],[80]
, with teams that work effectively providing higher quality care and patient safety[31]
. Healthcare students, including pharmacy students, are trained in profession-specific ways, yet are required to work in clinical settings as members of interprofessional teams[81]
. Pharmacists routinely need to collaborate with doctors to resolve and optimise prescribing outcomes. Effective communication skills are essential performance standards for UK pharmacists[82],[83]
, yet poor communication between healthcare professionals, including pharmacists and doctors, is considered a leading contributing factor of prescribing error[84]
.
While SBT is used within schools of pharmacy for dispensing, patient counselling, teaching of therapeutics and assessments in objective structured clinical examination, there is wider potential for clinical pharmacy to meet the evolving needs of the workforce. It could be used as a modality for training and assessment of clinical skills, application of pharmaceutical care, identification of medication errors, medicines reconciliation and prescribing tasks. As a technology, SBT has enhanced medical students’ knowledge and comfort in obtaining a medication history[85]
and similar benefits might be expected for pharmacists and pharmacy technicians who undertake this role in UK hospital settings.
This training can enhance the self-reported preparedness of pharmacists for high-stress clinical scenarios while on-call, including management of sepsis, stroke, epilepsy and bleeding[86]
. This demonstrates its potential application for enhancing knowledge and awareness of both frequent and rare clinical situations, or even to support pharmacists as they rotate between clinical areas and pharmacy placements, such as dispensary and medicines information.
Impact on patient safety
Medication errors are a leading cause of patient harm and can occur at the prescribing, dispensing or administration stages. Around 7% of prescribed items[87]
, 0.02–2.68% dispensed items[88]
and 3–8% of administered medications contain an error in the hospital setting. It has been estimated that up to 9% of hospital inpatients experience medicine-related harm[89]
, with many of these incidents being preventable. In addition, the cost of preventable harm from medicines has been estimated at more than £750m per year — a significant, avoidable expenditure[90]
.
Medication error causation is complex, with non-technical skills often described as contributing factors in both prescribing[91],[92],[93]
and administration errors[94]
. Failings in these non-technical skills have been estimated to contribute to 70–80% of errors in healthcare[29]
. The seminal report ‘To Err Is Human: Building a safer health system’, published in 1999, advocated simulation as a technique to educate on error management, reduce error and achieve a safer healthcare system[27]
. A more recent systematic review of the effect of SBT on medication errors also concluded that it can be effective at reducing risk of medication error[9]
.
As team training improves passenger safety in the aviation industry, multiprofessional team training can improve patient safety, with pharmacists actively involved in optimising medication outcomes. Here, SBT can be an effective tool at raising awareness of error and critical process[95]
, while reductions in medication administration errors by nurses have also been reported in a pharmacist-led patient simulation[96]
, with similar reductions in medication errors and improvements in patient outcomes reported from SBT elsewhere[31]
. Use of team training scenarios could enhance the non-technical skills of pharmacists to effectively communicate, work in a team, and influence and challenge medication issues while enhancing their clinical skills. These are integral skills in both foundation- and advanced-level competency frameworks for pharmacists[82],[83]
and SBT could provide the opportunity for pharmacists to develop the skills and attitudes required to both learn from, and prevent, error[97]
.
Challenges and limitations of SBT
SBT is not without limitations. It should be emphasised that it is a supplementary experience and not a replacement for clinical experience[5]
. More complex simulators and mannequins require tailored simulation facilities, technologies and resources. The cost of more sophisticated high-fidelity simulators can be considerable, with further associated costs for ongoing maintenance and ancillary equipment or materials[44],[73]
. Space to house a simulation suite is required, while staff skilled in the programming and use of the simulator, and assessment and debriefing of participants is also required, presenting limitations that are likely to be problematic for many pharmacy departments and organisations. The place and role of SBT in any clinical pharmacy curricula needs defining and should be aligned with relevant competencies, while SBT programmes will need further research and validation of their impact on both educational and clinical outcomes.
Such challenges will need to be overcome to enable SBT to be fully utilised in clinical pharmacy training. However, many hospitals and institutions already have access to these resources, and engagement with the dedicated clinical skills or simulation teams could foster a collaboration to support a dedicated or interprofessional SBT programme for pharmacists. Such collaboration could allow pharmacy faculties to develop and lead independently on their own SBT, creating opportunities to both drive the research agenda and contribute to the evidence base supporting SBT as a technique to help develop the skills of the pharmacy workforce.
Conclusion
SBT is an innovative and flexible training modality that is being increasingly used within healthcare to enhance quality and support attainment of professional competence. Effective training is critical for acquisition of the diverse skills required of healthcare professionals to deliver safe, high-quality care, and SBT can help develop and assess performance. Its use within clinical pharmacy has not evolved to the same levels as in other areas of healthcare; however, it offers clear potential not only for pharmacy-specific training, but for crew resource management training for entire clinical teams — along with potential benefits for optimising both medication and patient safety. As clinical pharmacy evolves to include more patient-facing roles, educators need to embrace educational interventions and technologies that will support the acquisition and development of the skills of tomorrow’s workforce; SBT is one option that should be explored further.
Useful resources
Pharmacists interested in developing or participating in simulation-based training (SBT) should contact their local clinical skills and simulation leads to explore potential for learning opportunities.
The following links provide additional information and support for those interested in exploring developing SBT further:
Financial and conflicts of interests disclosure
The authors have no relevant affiliations or financial involvement with any organisation or entity with a financial interest in or financial conflict with the subject matter or materials discussed in this manuscript. No writing assistance was used in the production of this manuscript.
Reading this article counts towards your CPD
You can use the following forms to record your learning and action points from this article from Pharmaceutical Journal Publications.
Your CPD module results are stored against your account here at The Pharmaceutical Journal. You must be registered and logged into the site to do this. To review your module results, go to the ‘My Account’ tab and then ‘My CPD’.
Any training, learning or development activities that you undertake for CPD can also be recorded as evidence as part of your RPS Faculty practice-based portfolio when preparing for Faculty membership. To start your RPS Faculty journey today, access the portfolio and tools at www.rpharms.com/Faculty
If your learning was planned in advance, please click: “Planned Learning”
If your learning was spontaneous, please click: “Unplanned Learning”
References
[1] Gallagher RM & Gallagher HC. Improving the working relationship between doctors and pharmacists: is inter-professional education the answer? Adv Health Sci Educ Pract 2012;17(2):247–257. doi: 10.1007/s10459-010-9260-5
[2] Gaba D. The future of simulation in health care. Qual Saf Health Care 2004;13(1):2–10. doi: 10.1136/qshc.2004.009878
[3] Aggarwal R, Mytton OT, Derbrew M et al. Training and simulation for patient safety. Qual Saf Health Care 2010;19(2):i34–43. doi: 10.1136/qshc.2009.038562
[4] Aggarwal R & Darzi A. Technical-skills training in the 21st century. N Engl J Med 2006;355:2695–2696. doi: 10.1056/NEJMe068179
[5] Dent JA & Harden RM. A practical guide for medical teachers. 3rd ed. Churchill Livingstone, London, 2009
[6] Crea K. Practice skill development through the use of human patient simulation. Am J Pharm Educ 2011;75(9):Article 188.
 doi: 10.5688/ajpe759188
[7] Lin K, Travlos DV, Wadelin JW et al. Simulation and introductory pharmacy practice experiences. Am J Pharm Educ 2011;75(10):Article 209. doi: 10.5688/ajpe7510209
[8] Seybert AL, Laughlin KK, Benedict NJ et al. Pharmacy student response to patient-simulation mannequins to teach performance-based pharmacotherapeutics. Am J Pharm Educ 2006;70(3):Article 48. doi: 10.5688/aj700348
[9] Sarfati L, Ranchon F, Vantard N et al. Human-simulation-based learning to prevent medication error: a systematic review. J Eval Clin Pract 2018;1–10. doi: 10.1111/jep.12883
[10] Carpenito LJ. Mandatory updating — a lifetime commitment. Nurs Times 1991;3;87(48):53–55. PMID: 1754457
[11] Curley LE, McDonald M & Aspden T. Use of a fictitious community-based virtual teaching platform to aid in the teaching of pharmacy practice skills: student perspectives after initial implementation. J Pharm Policy Pract 2016;9:24. doi: 10.1186/s40545-016-0077-3
[12] Hussainy SY, Styles K & Duncan G. A virtual practice environment to develop communication skills in pharmacy students. Am J Pharm Educ 2012;76(10):202. doi: 10.5688/ajpe7610202
[13] Damasio AR. The feeling of what happens: body and emotion in the making of consciousness. Harcourt Brace, New York, 1999
[14] Zigmont JJ, Kappus LJ & Sudikoff SN. Theoretical foundations of learning through simulation. Semin Perinatol 2011;35(2):47–51. doi: 10.1053/j.semperi.2011.01.002
[15] Wenger E. Communities of Practice: Learning, Meaning, And Identity (Learning in Doing: Social, Cognitive and Computational Perspectives). Cambridge University Press, Cambridge, UK, 2000
[16] Salas E, DiazGranados D, Klein C et al. Does team training improve team performance? A meta-analysis. Hum Factors 2008;50(6):903–933. doi: 10.1518/001872008X375009
[17] Eppich W, Howard V, Vozenilek J & Curran I. Simulation-based team training in healthcare. Simul Healthc 2011;6(7):S14–S19. doi: 10.1097/SIH.0b013e318229f550
[18] O’Daniel M, Rosenstein AH. Chapter 33: Professional communication and team collaboration. In: AHRQ. Patient Safety and Quality: An Evidenced-Based Handbook for Nurses. Agency for Healthcare Research and Quality, Maryland, 2008
[19] Daniels K & Auguste T. Moving forward in patient safety: multidisciplinary team training. Semin Perinatol 2013;37(3):146–150. doi: 10.1053/j.semperi.2013.02.004
[20] Fanning RM & Gabba DM. The role of debriefing in simulation-based learning. Simul Healthc 2007;2(2):115–125. doi: 10.1097/SIH.0b013e3180315539
[21] Knowles MS. The modern practice of adult education. From pedagogy to andragogy. Revised and updated ed. Follett, Illinois, 1980.
[22] Kolb DA. Experiential learning. Prentice-Hall, Michigan, 1984
[23] Lloyd M, Watmough S, O’Brien S et al. How to give and receive constructive feedback. Pharm J 2016;296(7887). doi: 10.1211/PJ.2016.20200756
[24] Reason JT. Human Error. Cambridge University Press, UK, 1990
[25] Moorthy K, Vincent C & Darzi A. Simulation based training. BMJ 2005;330:493. doi: 10.1136/bmj.330.7490.493
[26] Flin RH, O’Connor P & Crichton M. Safety at the sharp end: a guide to non-technical skills. Ashgate Publishing, Surrey, UK, 2008
[27] Kohn LT, Corrigan JM & Donaldson MS. To Err Is Human: Building a safer health system. National Academy Press, Washington DC, 1999
[28] Department of Health. An organisation with a memory. Report of an expert group on learning from adverse events in the NHS, chaired by the chief medical officer. The Stationery Office, London, 2000
[29] Salas E, Burke CS, Bowers CA et al. Team training in the skies: does crew resource management (CRM) training work? Hum Factors 2001;43(4):641–674. doi: 10.1518/001872001775870386
[30] Flin RH, O’Connor P & Crichton M. Safety at the sharp end: a guide to non-technical Skills. 2017 ed. Ashgate Publishing, Farnham, UK, 2017
[31] Lloyd M, Watmough SD, O’Brien SV et al. Exploring the impact of prescribing error feedback on prescribing behaviour: a qualitative study. Res Social Adm Pharm 2018;14(6):545–554. doi: 10.1016/j.sapharm.2017.06.010
[32] Weaver SJ, Dy SM & Rosen MA. Team-training in healthcare: a narrative synthesis of the literature. BMJ Qual Saf 2014;23(5):359–372. doi: 10.1136/bmjqs-2013-001848
[33] Prober CG & Khan S. Medical education reimagined: a call to action. Acad Med 2013;88(10):1407–1410. doi: 10.1097/ACM.0b013e3182a368bd
[34] Hawks SJ. The flipped classroom: now or never? AANA J 2014;82(4):264-269. PMID: 25167605
[35] Kachka P. Understanding the flipped classroom: Part 2. 2012. Available at: https://www.facultyfocus.com/articles/blended-flipped-learning/understanding-the-flipped-classroom-part-2/ (accessed September 2018)
[36] Moffett J. Twelve tips for ‘‘flipping’’ the classroom. Medical Teacher 2015;37(4):331–336. doi: 10.3109/0142159X.2014.943710
[37] Cavaco AM & Madeira F. European pharmacy students’ experience with virtual patient technology. Am J Pharm Educ 2012;76(6):Article 106. doi: 10.5688/ajpe766106
[38] Rosen KR. The history of medical simulation. J Crit Care 2008;23(2):157–166. doi: 10.1016/j.jcrc.2007.12.004
[39] Marken PA, Zimmerman C, Kennedy C et al. Human simulators and standardized patients to teach difficult conversations to interprofessional healthcare teams. Am J Pharm Educ 2010;74(7):Article 120. doi: 10.5688/aj7407120
[40] Smithson J, Bellingan M, Glass B & Mills J. Standardized patients in pharmacy education: an integrative literature review. Curr Pharm Teach Learn 2015;7(6):851–863. doi: 10.1016/j.cptl.2015.08.002
[41] Jones F, Passos-Neto CE & Braghiroli OFM. Simulation in medical education: Brief history and methodology. PPCR 2015;1(2):56–63. Available at: http://ppcr.org/journal/index.php/ppcrjournal/article/view/12/13 (accessed September 2018)
[42] Okuda Y, Bryson EO, DeMaria S et al. The utility of simulation in medical education: what is the evidence? Mt Sinai J Med 2009;76(4):330–343. doi: 10.1002/msj.20127
[43] Smith MA & Benedict N. Effectiveness of educational technology to improve patient care in pharmacy curricula. Am J Pharm Educ 2015;79(1):Article 15. doi: 10.5688/ajpe79115
[44] Douglass MA, Casale JP, Skirvin JA & DiVall MV. A virtual patient software program to improve pharmacy student learning in a comprehensive disease management course. Am J Pharm Educ 2013;77(8):Article 172. doi: 10.5688/ajpe778172
[45] Benedict N & Schonder K. Patient simulation software to augment an advanced pharmaceutics course. Am J Pharm Educ 2011;75(2):Article 21. doi: 10.5688/ajpe75221
[46] Cook DA. One drop at a time: research to advance the science of simulation. Simul Healthc 2010;5(1):1–4. doi: 10.1097/SIH.0b013e3181c82aaa
[47] Pranaat R, Mohan V, O’Reilly M et al. Use of simulation based on an electronic health records environment to evaluate the structure and accuracy of notes generated by medical scribes: proof-of-concept study. JMIR 2017;5(3):e30. doi: 10.2196/medinform.7883
[48] Gillette C, Stanton RB, Rockich-Winston N et al. Cost-effectiveness of using standardized patients to assess student-pharmacist communication skills. Am J Pharm Educ 2017;81(10):Article 6120. doi: 10.5688/ajpe6120
[49] Vyas D, Bray BS & Wilson MN. Use of simulation-based teaching methodologies in US colleges and schools of pharmacy. Am J Pharm Educ 2013;77(3):Article 53. doi: 10.5688/ajpe77353
[50] Bradley P. The history of simulation in medical education and possible future directions. Med Educ 2006;40(3):254–262. doi: 10.1111/j.1365-2929.2006.02394.x
[51] Rudolph JW, Simon R, Rivard P et al. Debriefing with good judgment: combining rigorous feedback with genuine inquiry. Anesthesiol Clin 2007;25(2):361–376. doi: 10.1016/j.anclin.2007.03.007
[52] Motola I, Devine LA, Chung HS & Issenberg SB. Simulation in healthcare education: a best evidence practical guide. AMEE guide no. 82. Med Teach 2013;35(10):e1511–e1530 doi: 10.3109/0142159X.2013.818632
[53] Eppich W & Cheng A. Promoting excellence and reflective learning in simulation (PEARLS): development and rationale for a blended approach to health care simulation debriefing. Simul Healthc 2015;10(2):106–115. doi: 10.1097/SIH.0000000000000072
[54] Riley RH. Manual of simulation in healthcare. 2nd ed. Oxford University Press, Oxford, UK, 2015
[55] Eppich W & Cheng A. How cultural-historical activity theory can inform interprofessional team debriefings. Clin Sim Nurs 2015;11(8):383–389. doi: 10.1016/j.ecns.2015.05.012
[56] Watmough S, Box H, Bennett N et al. Unexpected medical undergraduate simulation training (UMUST): can unexpected medical simulation scenarios help prepare medical students for the transition to foundation year doctor? BMC Med Educ 2016;16:110. doi: 10.1186/s12909-016-0629-x
[57] Kolbe M, Weiss M, Grote G et al. TeamGAINS: a tool for structured debriefings for simulation-based team trainings. BMJ Qual Saf 2013;22(7):541–553. doi: 10.1136/bmjqs-2012-000917
[58] Hollnagel E, Wears RL & Braithwaite J. From safety-I to safety-II: a white paper. National Library of Congress, Washington DC. doi: 10.13140/RG.2.1.4051.5282
[59] Dieckmann P, Patterson M, Lahlou S et al. Variation and adaptation: learning from success in patient safety-oriented simulation training. Adv Simul (Lond) 2017;2:21. doi: 10.1186/s41077-017-0054-1
[60] Staender S. Safety-II and resilience: the way ahead in patient safety in anaesthesiology. Curr Opin Anaesthesiol 2015;28(6):735–739. doi: 10.1097/ACO.0000000000000252
[61] Ellis S & Davidi I. After-event reviews: drawing lessons from successful and failed experience. J Appl Psychol 2005;90(5):857–871. doi: 10.1037/0021-9010.90.5.857
[62] Schmutz JB, Kolbe M & Eppich WJ. Twelve tips for integrating team reflexivity into your simulation-based team training. Medical Teacher 2018;40(7):721–727. doi: 10.1080/0142159X.2018.1464135
[63] Pauly-O’Neill S. Beyond the five rights: Improving patient safety in pediatric medication administration through simulation. Clin Simul Nurs 2009;5(5):e181–e186.
 doi: 10.1016/j.ecns.2009.05.059
[64] Cant RP & Cooper SJ. Simulation-based learning in nurse education: systematic review. J Adv Nurs 2010;66(1):3–15.
 doi: 10.1111/j.1365-2648.2009.05240.x
[65] Norman J. Systematic review of the literature on simulation in nursing education. ABNF J. 2012;23(2):24–28. PMID: 75292183
[66] Aebersold M. The history of simulation and its impact on the future. AACN Adv Crit Care 2017;27(1):56–61. doi: 10.4037/aacnacc2016436
[67] Hayden JK, Smiley RA, Alexander M et al. The NCSBN National Simulation Study: a longitudinal, randomized, controlled study replacing clinical hours with simulation in prelicensure nursing education. J Nurs Regul 2014;5(2):S3–S40. doi: 10.1016/S2155-8256(15)30062-4
[68] Branch C. Pharmacy students’ learning and satisfaction with high-fidelity simulation to teach drug-induced dyspepsia. Am J Pharm Educ 2013;77(2):Article 30. doi: 10.5688/ajpe77230
[69] Reape A, Lips-Nassif C, Bailey L et al. The use of human patient simulators for teaching UK pharmacy students about critical care. Pharm Educ 2011;11(1):1–7. Available at: http://pharmacyeducation.fip.org/pharmacyeducation/article/view/340 (accessed September 2018)
[70] Regan K, Harney L, Goodhand K et al. Pharmacy simulation: a Scottish, student-led perspective with lessons for the UK and beyond. Pharmacy 2014;2(1):50–64. doi: 10.3390/pharmacy2010050
[71] Langley C, Jesson J & Wilson K. Learning with other health professions in the United Kingdom MPharm degree: multidisciplinary and placement education. Pharm Educ 2010;10(1):39–46.
[72] Smith A & Darracott R. Modernising Pharmacy Careers Programme. Review of pharmacist undergraduate education and pre-registration training and proposals for reform. Report to Medical Education England Board. 2011. Available at: http://docplayer.net/26553607-Modernising-pharmacy-careers-programme-review-of-pharmacist-undergraduate-education-and-pre-registration-training-and-proposals-for-reform.html (accessed September 2018)
[73] Seybert AL. Patient simulation in pharmacy education. Am J Pharm Educ 2011;75(9):Article 187. doi: 10.5688/ajpe759187
[74] Vyas D, Ottis EJ & Caligiuri FJ. Teaching clinical reasoning and problem-solving skills using human patient simulation. Am J Pharm Educ 2011;75(9):Article 189. doi: 10.5688/ajpe759189
[75] Seybert AL & Barton CM. Simulation-based learning to teach blood pressure assessment to doctor of pharmacy students. Am J Pharm Educ 2007;71(3):Article 48. doi: 10.5688/aj710348
[76] Seybert AL & Kane-Gill SL. Elective course in acute care using online learning and patient simulation. Am J Pharm Educ 2011;75(3):Article 54. doi: 10.5688/ajpe75354
[77] Mieure KD, Vincent WR, Cox MR et al. A high-fidelity simulation mannequin to introduce pharmacy students to advanced cardiovascular life support. Am J Pharm Educ 2010;74(2):Article 22. doi: 10.5688/aj740222
[78] Bernaitis N, Baumann-Birkbeck L, Alcorn S et al. Simulated patient cases using DecisionSimâ„¢ improves student performance and satisfaction in pharmacotherapeutics education. Curr Pharm Teach Learn 2018;10(6):730–735. doi: 10.1016/j.cptl.2018.03.020
[79] Tokunaga J, Takamura N, Ogata K et al. Vital sign monitoring using human patient simulators at pharmacy schools in Japan. Am J Pharm Educ 2010;74(7):Article 132. doi: 10.5688/aj7407132
[80] Fernandez R, Parker D, Kalus JS et al. Using a human patient simulation mannequin to teach interdisciplinary team skills to pharmacy students. Am J Pharm Educ 2007;71(3):Article 51.
 doi: 10.5688/aj710351
[81] Thomson K, Outram S, Gilligan C & Levett-Jones T. Interprofessional experiences of recent healthcare graduates: a social psychology perspective on the barriers to effective communication, teamwork, and patient-centred care. J Interprof Care 2015;29(6):634–640. doi: 10.3109/13561820.2015.1040873
[82] Royal Pharmaceutical Society. The RPS foundation pharmacy framework. A framework for professional development in foundation practice across pharmacy. 2014. Available at: https://www.rpharms.com/Portals/0/RPS%20document%20library/Open%20access/Frameworks/RPS%20Foundation%20Pharmacy%20Framework.pdf (accessed September 2018)
[83] Royal Pharmaceutical Society. The RPS advanced pharmacy framework (APF). 2013. Available at: https://www.rpharms.com/Portals/0/RPS%20document%20library/Open%20access/Frameworks/RPS%20Advanced%20Pharmacy%20Framework.pdf (accessed September 2018)
[84] Dornan T, Ashcroft D, Heathfield H et al. An in-depth investigation into causes of prescribing errors by foundation trainees in relation to their medical education — EQUIP Study. 2009. Available at: http://www.gmc-uk.org/FINAL_Report_prevalence_and_causes_of_prescribing_errors.pdf_28935150.pdf (accessed September 2018)
[85] Lindquist LA, Gleason KM, McDaniel MR et al. Teaching medication reconciliation through simulation: a patient safety initiative for second year medical students. J Gen Intern Med 2008;23(7):998–1001. doi: 10.1007/s11606-008-0567-3
[86] Thomson Bastin ML, Cook AM & Flannery AH. Use of simulation training to prepare pharmacy residents for medical emergencies. Am J Health-Syst Pharm 2017;74(6):424–429. doi: 10.2146/ajhp160129
[87] Lewis PJ, Dornan T, Taylor D et al. Prevalence, incidence and nature of prescribing errors in hospital inpatients: a systematic review. Drug Safety 2009;32(5):379–389. doi: 10.2165/00002018-200932050-00002
[88] James KL. Barlow D, Mcartney R et al. Incidence, type and causes of dispensing errors: review of the literature. In J Phar Pract 2009;17(1):9–30. doi: 10.1211/ijpp.17.1.0004
[89] Davies EC, Green CF, Mottram DR & Pirmohamed M. Adverse drug reactions in hospital inpatients: a pilot study. J Clin Pharm Ther 2006;31(4):335–341. doi: 10.1111/j.1365-2710.2006.00744.x
[90] National Patient Safety Agency. Safety in doses: improving the use of medicines in the UK. 2007
[91] Ryan C, Ross S, Davey P et al. Prevalence and Causes of Prescribing Errors: The Prescribing Outcomes for Trainee Doctors Engaged in Clinical Training (PROTECT) Study. PLoS ONE 2014;9(1):e79802. doi: 10.1371/journal.pone.0079802
[92] Ross S, Bond C, Rothnie H et al. What is the scale of prescribing errors committed by junior doctors? A systematic review. Br J Clin Pharmacol 2009;67(6):629–640. doi: 10.1111/j.1365-2125.2008.03330.x
[93] Lewis P, Ashcroft DM, Dornan T et al. Exploring the causes of junior doctors’ prescribing mistakes: a qualitative study. Br J Clin Pharmacol 2014;78(2):310–319. doi: 10.1111/bcp.12332
[94] Keers RN, Williams SD, Cooke J et al. Causes of medication administration errors in hospitals: a systematic review of quantitative and qualitative evidence. Drug Safety 2013;36(11):1045–1067. doi: 10.1007/s40264-013-0090-2
[95] Daupin J, Atkinson S, Bédard P et al. Medication errors room: a simulation to assess the medical, nursing and pharmacy staffs’ ability to identify errors related to the medication-use system. J Eval Clin Pract 2016;22(6):911–920. doi: 10.1111/jep.12558
[96] Ford DG, Seybert AL, Smithburger PL et al. Impact of simulation-based learning on medication error rates in critically ill patients. Intens Care Med 2010;36(9):1526–1531.
 doi: 10.1007/s00134-010-1860-2
[97] Ziv A, Ben-David S & Ziv M. Simulation based medical education: an opportunity to learn from errors. Med Teach 2005;27(3):193–199. doi: 10.1080/01421590500126718