This content was published in 2004. We do not recommend that you take any clinical decisions based on this information without first ensuring you have checked the latest guidance.
Most pharmacists will be familiar with the “pin-prick” used to obtain a few drops of blood from a finger tip or earlobe to measure blood-glucose levels. For other blood tests, blood is usually drawn from the median vein in the antecubital fossa (area in front of the elbow), after applying a tourniquet to the upper arm. Typically, a 10 or20ml syringe is used, but the amount of blood collected will depend on the tests requested and the number of sample tubes to be filled. For blood gases, arterial blood (drawn at the wrist) is required and the procedure is usually more painful than venous blood collection.
Full blood count
The most commonly requested blood test is the full blood count (FBC), which includes an assessment of the number, size and appearance of the three cellular elements in blood: erythrocytes (red cells), leucocytes (white cells) and thrombocytes (platelets). It can, therefore, be used to detect anaemia, leukaemia, blood clotting problems and many other conditions. Typical parameters with their reference ranges are shown in Panel 1(p420) and are described below. It should be noted that reference ranges can vary, depend-ing on the laboratory used.
Red blood cell tests
Tests relating to erythrocytes are used primarily to diagnose and investigate the possible causes of anaemia.
Red cell count
The red cell count (RCC) is decreased in anaemia and raised in dehydration. A high RCC also indicates polycythaemia (abnormal increase in erythrocyte production by the bone marrow).
Identify knowledge gaps
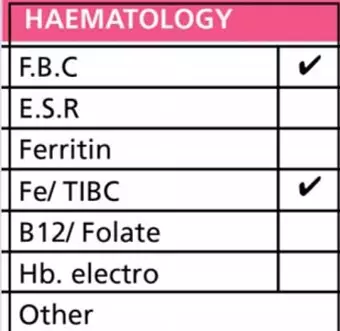
1. Look at the section of the pathology request form, pictured above. Do you know what all the tests are?
2. What parameters does an FBC look at?
3. What kinds of conditions are suggested by a high ESR?
Before reading on, think about how this article may help you to do your job better. The Royal Pharmaceutical Society’s areas of competence for pharmacists are listed in “Plan and record”, (available at: www.rpsgb.org/education). This article relates to “diagnostic tests” and “therapeutic drug monitoring” (see appendix 4 of “Plan and record”).
Packed cell volume and mean cell volume
The packed cell volume (PCV) or “haematocrit” is the percentage of the total blood volume occupied by red cells. Traditionally, this has been determined by centrifuging blood in a microhaematocrit tube and measuring the height of the red cell column, but now auto-mated analysers are used to calculate PCV. Centrifuging causes the components of the blood to separate. Red cells move to the bottom of the tube and plasma to the top, with a “buffy coat” (which contains leucocytes and platelets) in the middle. The appearance of the centrifuged sample can also provide subjective information about the patient’s health. For example, the colour and clarity of the plasma can suggest jaundice (dark plasma) or lipaemia (turbid plasma).
PCV can be used as a screening tool for anaemia and to indicate the degree of fluid loss in dehydration. A drop in PCV can also indicate internal haemorrhage before any other symptoms become apparent. PCV is raised in polycythaemia and in chronic hypoxia associated with pulmonary disease and congenital heart disease.
Mean cell volume (MCV) is the average volume of a red blood cell, measured in femtolitres. It can be calculated using the following equation: MCV=PCV/RCC.
A raised MCV suggests folate or vitamin B12 deficiency, myxoedema, alcoholism or liver disease, haemolysis or aplasia. A reduced MCV suggests chronic blood loss, iron deficiency anaemia, thalassaemia or sideroblastic anaemia.
Haemoglobin and mean cell haemoglobin concentration
About a third of each erythrocyte is haemoglobin. One way of measuring haemoglobin concentration is to add a lysing agent to a sample of diluted blood so that the red cells release their haemoglobin. This can be converted to cyanomethaemoglobin and a spectrophotometer can then be used to measure optical density, from which haemoglobin concentration can be calculated. Reference ranges for haemoglobin are shown in Panel 1.
Panel 1: Typical full blood count reference ranges
- RCC (red cell count): 4.5–6.5 x 1012/L (male); 3.9–5.6 x 1012/L (female)
- PCV (packed cell volume or haematocrit): 0.4–0.54 (male); 0.37–0.49 (female)
- MCV (mean cell volume): 80–100 fL
- Hb (haemoglobin): 13.5–17.5g/dl (male); 11.5–15.5g/dl (female)
- MCHC (mean cell haemoglobin concentration): 30–36 g/dl
- WCC (white cell count): 4.0–11.0 x 109/L
- Neutrophil count (40–75 per cent WCC): 0.5–7.5 x 109/L
- Lymphocyte count(20–40 per cent WCC): 1.5–4.9 x 109/L
- Monocyte count(2–10 per cent WCC): 0.2–0.8 x 109/L
- Eosinophil count(1–5 per cent WCC): 0.04–0.44 x 109/L
- Basophil count(<1 per cent WCC): 0.01–0.10 x 109/L
- Platelet count: 150–400 x 109/L
- PT (prothrombin time)(factors I, II, VII, X): 10–14 seconds
- APTT (activated partial thromboplastin time)(VIII, IX, XI, XII): 35–45 seconds
- Thrombin time: 14–16 seconds
- ESR (erythrocyte sedimentation rate, Wintrobe method): <10mm/h (male); <20mm/h (female)
Concentrations of haemoglobin are reduced in anaemia. They areraised in polycythaemia, hypoxia, renal conditions where excess erythropoietin is produced and dehydration. Smoking can raise haemoglobin measures due to increased carboxy-haemoglobin.
The mean cell haemoglobin concentration (MCHC) is a measure of the average concentration of haemoglobin in red cells. A reduced MCHC suggests iron deficiency or chronicblood loss.
White blood cell tests
An increase in the leucocyte count (leucocytosis) occurs most commonly as a result of infection, inflammation or any major tissue damage. However, in people with cancers, such as leukaemia, there are large increases. A reduction in white cell concentration (leucopenia) is far less common than an increase. However, leucocytosis can be benign whereas leucopenia always indicates a health problem. Chemotherapy decreases white blood cell counts.
White cell counts outside the reference range are the result of an increase or decrease in one or more of the five types of leucocyte: neutrophils, eosinophils, basophils, lymphocytes and monocytes. White cell counts are usually done by an automated instrument. The blood sample is mixed with a chemical to break the red blood cells and the remaining white cells are counted by the instrument. Different white cells are identified and counted by spreading a drop of blood onto a slide, staining it and examining the slide under a microscope. One-hundred white cells are counted (including any atypical or immature cells). Cells are identified by the shape and appearance of their nucleus, the colour of cytoplasm and the presence of granules.
Neutrophils
An increased neutrophil count (neutrophilia) is a feature of most acute bacterial infections, acute inflammatory conditions (eg, rheumatoid arthritis), pregnancy, surgery, burns, myocardial infarction and solid tumours (eg, lung cancer). A low neutrophil count (neutropenia) is a feature of some viral infections (eg, mumps, influenza, human immunodeficiency virus, viral hepatitis),aplastic anaemia, acute leukaemia and some advanced cancers (particularly tumours that have spread to the bone).
Eosinophils
A raised eosinophil count (eosinophilia) may be caused by allergic conditions (eg, hay fever), allergic drug reactions and parasitic worm infections.
Basophils
“Abnormal” counts of basophil cells are rare, but numbers are raised in patients with chronic myeloid leukaemia.
Lymphocytes
A high lymphocyte count (lymphocytosis) is a typical feature of glandular fever. Lymphocytosis can also occur in patients in the early stages of HIV infection, viral hepatitis, mumps, rubella, chickenpox, tuberculosis and whooping cough. A reduced lymphocyte count is associated with acquired immune deficiency syndrome, systemic lupus erythmatosus, influenza, burns and surgery.
Monocytes
An increased monocyte count (monocytosis) can occur in patients with tuberculosis, subacute bacterial endocarditis and other chronic bacterial infections.
Platelet count
Platelets can be counted manually by diluting samples and using a haemocytometer (a glass slide with a ruled counting chamber) and a microscope. However, this method is inaccurate compared with using an automated counter (eg, a haematology analyser). Aggregated platelets invalidate the count. Platelet numbers can also be estimated by examining a stained blood film. No count is performed, but the number is judged as “increased” (above reference intervals), “adequate” (within reference intervals), “low” or “very low”.
A reduced platelet count (thrombocytopenia) is a feature of immune thrombocytopenic purpura (visible haemorrhages into the skin and mucous membranes). It can also be caused by drugs, such as some antibiotics (eg, penicillin, sulphonamides), some diuretics (eg, furosemide, acetazolamide) and some anti-inflammatories.
A large increase in platelet concentration can occur in malignant disorders of the bone marrow, characterised by abnormal proliferation of myeloid stem cells (eg, chronic myeloid leukaemia). A mild to moderate increase is more common and can be seen in severe infectious illness (eg, septicaemia),chronic inflammatory conditions (eg, rheumatoid arthritis), as well as after haemorrhage, surgery or other severe trauma.
Erythrocyte sedimentation rate
Erythrocyte sedimentation rate (ESR) is found by putting a blood sample into an ESR tube and timing how long it takes for erythrocytes to fall to the bottom, at room temperature. The erythrocytes of healthy people do not fall far down the narrow tube. However, in diseases where abnormal or extra proteins are made, erythrocytes aggregate —they are heavier and fall faster. Two main test methods (Westergren and Wintrobe) are used by laboratories and each has different reference ranges. Results can also depend on age and sex.
ESR is a non-specific test — it only suggests possible illnesses, particularly those involving inflammation. ESR is also raised in injury and malignancy. However, in most of these conditions, it is possible for ESR to be normal. In clinical practice, ESR is used as supportive evidence of conditions such as rheumatoid arthritis, Crohn’s disease and ulcerative colitis. It can also be used to monitor the effectiveness of therapy in those suffering from a chronic infection (eg, tuberculosis and subacute bacterial endocarditis). Measuring ESR has no place in the diagnosis of cancer, with the exception of multiple myeloma where raised ESRs are found so consistently that this is one of the diagnostic criteria for the condition. In addition, ESR is raised in Hodgkin’s disease, where the test is used not for diagnostic purposes but for monitoring the progress of the disease and the effectiveness of therapy.
Ferritin and folate
About 30 per cent of the iron in the body is stored as ferritin in the bone marrow, spleen and liver. The amount of ferritin in serum is directly proportional to the amount of iron in the body. Serum ferritin levels are, therefore, measured to diagnose iron deficiency anaemia. The usual range is 24–300ng/L for men and15–300ng/L for women.
Low serum ferritin levels are seen in patients with iron deficiency and in women who suffer heavy menstrual bleeds. Increased serum ferritin levels are seen in hyperthyroidism, Hodgkin’s lymphoma and breast cancer.
Another test often requested is serum folate (or vitamin B12). Usual levels range between 2 and 10ng/ml. Folate levels are used to indicate pernicious anaemia or intestinal malabsorption disorders (eg, Crohn’s disease),but decreased levels are also seen in people with chronic alcoholism. Suspected impairedB12absorption can be investigated using the Schilling test. This involves giving the patient radioactive vitamin B12and collecting urine samples over a number of days.
Iron and total iron binding capacity
Iron is transported around the body by transferrin molecules (each can carry two iron atoms). Total iron binding capacity (TIBC) is usually requested when iron deficiency anaemia is suspected. Iron is added to a blood sample to saturate transferrin and the amount of iron bound represents TIBC. A low saturation means that there is a high proportion of vacant binding sites. Patients are asked to fast for eight hours before blood is collected. Serum iron is usually also measured at the same time as TIBC. Normal serum iron and TIBC values are 10–30μmol/L and40–75μmol/L, respectively. Low iron levels can suggest chronic blood loss or inadequate absorption of iron from t he diet. Low TIBC values can suggest cirrhosis or pernicious or haemolytic anaemia.
Action: practice points
Reading is only one way to undertake CPD and the Society will expect to see various approaches in a pharmacist’s CPD portfolio.
1. Improve your knowledge of any of the conditions mentioned in this article, eg, thalassaemia or myxoedema.
2. Read under the “Dose” and “Monitoring” headings in section 2.8.2 (Oral anticoagulants) of the British National Formulary.
3. Learn more about blood gases. For example, use the free tutorial manual, available at: www.madsci.com
Evaluate
For your work to be presented as CPD, you need to evaluate your reading and any other activities. Answer the following questions: What have you learnt? How has it added value to your practice? (Have you applied this learning or had any feedback?) What will you do now and how will this be achieved?
Haemoglobin electrophoresis
Haemoglobin electrophoresis (Hb electro) can be used to detect other types of anaemia. Electrophoresis is used to separate charged particles by applying an electric current to a solution. Haemoglobin electrophoresis allows the different types of haemoglobin in a blood sample to be detected and measured. It is used to diagnose sickle cell anaemia (by detecting HbS, a type of haemoglobin) and thalassaemia.
Gammaglobulins
Electrophoresis can also be performed on serum to detect the presence of monoclonal and polyclonal immunoglobulins in theblood. Usually, no monoclonal antibodies are detected in a healthy per son, and their presence can indicate a malignant disorder.
Blood coagulation tests
Essentially, blood coagulation tests measure the time taken for a sample of patient’s blood plasma to form a fibrin clot in a test tube after addition of a reagent that initiates the clotting cascade. There are three main coagulation tests, each relevant to different clotting factors. The tests are often done together because different combi-nations of results (eg, high APTT but normal PT)indicate different conditions.
Prothrombin time
Prothrombin time (PT) is usually between 10 and14 seconds. Commercially produced thromboplastin (factor III) is added to plasma and the time taken in seconds for the plasma to clot is determined. The test is sensitive to reduced levels of factors V, VII and X, prothrombin and fibrino-gen. Deficiency of one of more of these factors will result in an abnormally long time for a fibrin clot to form (ie, PT will be increased). PT is also used to monitor oral anticoagulants.
Activated partial thromboplastin time
Also known as kaolin cephalin clotting time (KCCT), activated partial thromboplastin time (APTT) can be related to the intrinsic clotting cascade. An abnormally prolonged APTT indicates a deficiency of one or moreof factors VIII, IX, XI or XII. This test is used for monitoring intravenous heparin.
Thrombin time
To find thrombin time (TT) thrombin is added to a plasma sample. The test specifically looks at the final stage of the coagulation pathway — conversion of fibrinogen to fibrin. An abnormally long TT indicates deficiency of factor I (fibrinogen).
International normalised ratio
The international normalised ratio (INR) uses PT to measure the effect of oral anticoagulant drugs. It is the ratio of a patient’s prothrombin time to the mean normal prothrombin time in a group of healthy subjects, exponentially standardised by the international sensitivity index (ISI) of the reagent or instrument combination used:
INR =Patient’s prothrombin time/Mean normal prothrombin time
Reported INR results are, therefore, independent of the reagents and methods used. Initially, INR is checked daily or on alternate days after starting therapy. After hospital discharge INR is generally measured every week for four to six weeks, and up to every 12 weeks if control and compliance are satisfactory. Changes in a patient’s medical condition (eg, heart disease, thyroid status) or drug therapy (eg, a broad- spectrum antibiotic is prescribed) can alter anticoagulant control and more frequent monitoring may be required.
Patients not on anticoagulant therapy, have an INR of 1. INR values in properly anticoagulated patients will range between 2.0 and 3.5, depending on the condition being managed. Full details and target INRs currently recommended by the British Society for Haematology can be found in the British National Formulary.
Blood gases
The test for blood gases includes the measurement of oxygen (pO2), carbon dioxide (pCO2) and blood pH together with other parameters of acid-base balance, such as the concentration of bicarbonate. Normal adult reference ranges for partial pressures of oxygen and carbon dioxide are 10.6–13.3kPa(80–100mmHg) and 4.5–6.0kPa (35–45mmHg), respectively. Blood pH is usually between 7.35 and 7.4 and bicarbonate levels are usually between 22 and 28mmol/L. Acid-base disturbances can be classified as either acidosis or alkalosis.
pO2, pCO2, and pH are all affected by a change in a patient’s temperature so readings may need to be adjusted accordingly. Blood gases are assessed (usually using chemoluminescence techniques) in order to monitor critically ill patients (eg, checking cardiopulmonary function and acid-base balance). If blood gas measurements are required every few hours an arterial line is used. Reasons for low pO2 include hypoventilation and alveolar-capillary block. High pO2 can be seen with hyperventilation or oxygen therapy. Low pCO2 (respiratory alkalosis) is usually a compensatory phenomenon in metabolic acidosis, but may be a primary abnormality; in both situations it is due to hyperventilation. Increased pCO2 (respiratory acidosis) commonly occurs in respiratory failure.
Urea and electrolytes
Urea and electrolytes (U&Es) in the blood are also measured. This test can be performed as a general health check (a test called “Chem 7”,available in the US measures urea, sodium, potassium, chloride, creatinine, bicarbonate and also glucose) but is also an indication of kidney or lung function and hydration levels. For example, high urea, chloride and creatinine levels point to renal failure. Measuring U&Es can be used to monitor the effects of drug therapy or the general state of hospital patients (eg, monitoring patients with diabetes who are at risk of hyperkalaemia), so that rapid corrective action can be taken if necessary.
Pamela Mason, PhD, MRPharmS, is a freelance journalist and author, based in Monmouthshire

