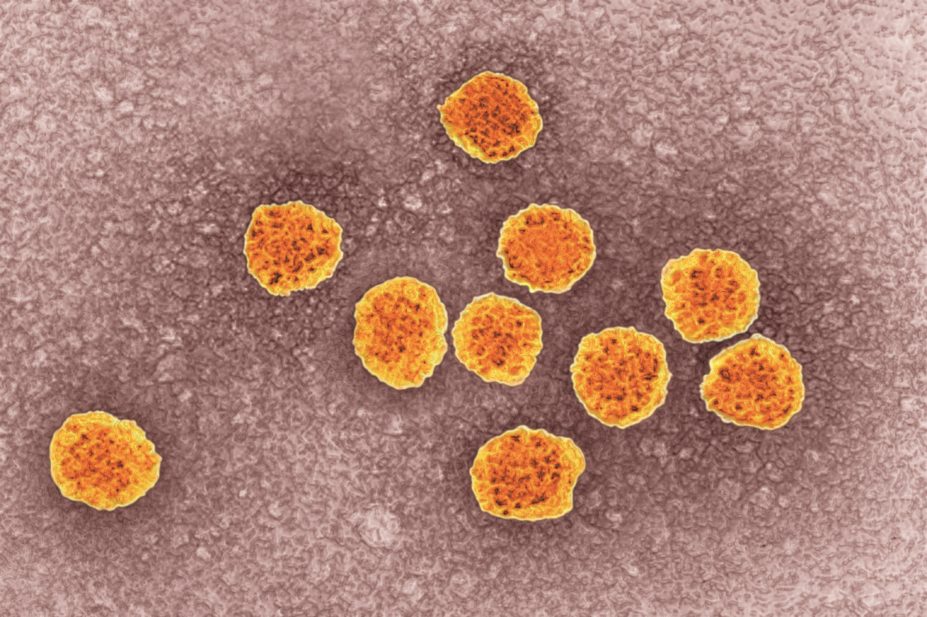
BSIP SA / Alamy
An anti-allergy treatment is effective in treating hepatitis C virus (HCV), a study has found, raising hopes of an affordable weapon in the fight against the virus.
The antihistamine, chlorcyclizine hydrochloride, prevents an early stage of HCV infection, most likely by targeting viral entry into host cells, according to research published in Science Translational Medicine
[1]
on 8 April 2015.
Using a cell-based quantitative high-throughput platform, the scientists tested a number of drugs that were already approved by the US Food and Drug Administration (FDA) for their efficacy against HCV.
The team, which included researchers from the US National Institutes of Health (NIH) and Hiroshima University in Japan, found that chlorcyclizine strongly inhibited HCV infection in human hepatoma cells and primary human hepatocytes. The antihistamine significantly inhibited infection of HCV genotypes 1b and 2a without substantial toxicity or evidence of drug resistance during four and six weeks of treatment, respectively.
The researchers noted that a number of FDA-approved drugs, including the anticancer agents erlotinib and dasatinib, the cholesterol lowering therapy ezetimibe and the antimalarial drug ferroquine, have shown anti-HCV activities, however, chlorcyclizine showed more compelling in vitro and in vivo activity against HCV infection than the others.
Because the data is based only on laboratory and mouse models, it is too soon to say if chlorcyclizine could cure patients of the virus, according to Jake Liang, head of the liver disease branch of the National Institute of Diabetes and Digestive and Kidney Diseases at the NIH, and a lead author of the study. He said that chlorcyclizine would most likely have to be used in combination with existing HCV treatments in order to be most effective.
The researchers found that chlorcyclizine’s antiviral effect was “synergistic” with other anti-HCV drugs — including ribavirin, interferon-alpha, telaprevir, boceprevir, sofosbuvir, daclatasvir and cyclosporin A — without producing significant cytotoxicity, indicating it could be used in tandem with established HCV treatments. They also noted that combination regimens for treating chronic HCV infection “lower the chance of developing drug-resistant viral mutations”.
The discovery represents a potentially profound breakthrough in the search for effective and affordable treatments for HCV, which affects around 185 million people around the world and for which there is no vaccine. The virus, which is especially prevalent in Africa and Asia, as well as in high-risk populations such as intravenous drug users, can often remain undetected for many years and can cause cirrhosis of the liver or liver cancer in those with chronic infection.
While pegylated interferon and ribavirin has been the standard treatment for a number of years, the discovery of direct-acting antivirals have raised hopes of reducing the health and financial burden caused by the disease, but have also raised questions about affordability. Although some of these newer drugs have been shown to cure HCV in up to 90% of those infected, Solvadi (sofosbuvir), one of the latest treatments, costs around US$84,000 for 12 weeks of therapy, making it inaccessible to many.
“The repurposing or repositioning of [chlorcyclizine] in HCV treatment may provide a more affordable alternative to the current costly options, especially in low-resource settings where chronic HCV infection is endemic,” the study says. Chlorcyclizine costs US$0.55 per tablet.
Liang said chlorcyclizine could be used in people with all stages of HCV infection, but could be particularly helpful to patients with advanced disease who are undergoing liver transplants. Noting that the drug blocks entry of the virus into cells, Liang added, “this drug can be used theoretically to prevent re-infection during transplantation surgery”.
Because chlorcyclizine is known to cross the blood-brain barrier and cause side effects such as sedation, the researchers said central nervous system penetration of the drug would need to be taken into consideration for future development.
References
[1] He S, Lin B, Chu V et al. Repurposing of the antihistamine chlorcyclizine and related compounds for treatment of hepatitis C virus infection. Science Translational Medicine 2015. doi: 10.1126/scitranslmed.3010286.
You may also be interested in

Genomics surveillance programme for hepatitis C launched by UK Health Security Agency

How we treated more than 100 hepatitis C patients at pharmacist-led clinics in North Wales
