Shutterstock.com
Past several swipe-lock doors, down a flight of stairs and through a rabbit warren of dimly lit corridors, Francis Lévi walks hurriedly to his office in the University of Warwick’s medical school in Coventry, West Midlands. Lévi is on a mission: he wants to find out whether the time of day a cancer patient receives a particular drug affects treatment toxicity or efficacy. And if it does, is there an optimal time to treat a patient?
Lévi, a medical oncologist and biomedical scientist, has been probing the potential of so-called chronotherapy in cancer for more than 20 years. As the human body is governed by biological rhythms, the thinking is that a drug’s effectiveness and toxicity can be influenced by the exact time it is given. In experiments in mice, Lévi has shown that the tolerability and effectiveness of chemotherapy varies at different times of the day and night. By using mathematical models he can predict the optimal time at which to give an animal a drug to maximise its effectiveness and tolerability.
By timing administration right you can increase a drug’s effectiveness and simultaneously make it less toxic to the patient
“It’s against the classic chemotherapy paradigm,” explains Lévi excitedly as we reach his office. With traditional dose-escalation methods, incremental increases in dose and efficacy are capped by unacceptable toxicity. “It’s the opposite with chronotherapy — by timing administration right you can increase a drug’s effectiveness and simultaneously make it less toxic to the patient.”

Source: Dara Mohammadi
Francis Lévi, oncologist and biomedical scientist at the University of Warwick, says timing administration right can increase a drug’s effectiveness and simultaneously make it less toxic to the patient
The body’s circadian rhythm, or biological clock, runs over a period of around 24 hours and affects not only sleep patterns but immune function and metabolism. In response to environmental cues, such as light, a region of the hypothalamus called the suprachiasmatic nucleus sends out neuronal and hormonal signals that coordinate a molecular clock within every cell. These cellular clocks are driven by the oscillating and interacting expression of at least 14 genes, known as the core clock genes.
The premise of chronobiology is that the molecular clock in cancer cells tends to be out of sync with the clocks in healthy cells. It’s a finding observed as early as 1966 by US researchers investigating mitotic cycles in human breast and skin cancer cells[1]
, and one explained mechanistically in 2006 when Lévi showed the expression of clock genes Rev-erbα, Per2, and Bmal1 differed between cancerous and healthy liver cells in mice[2]
.
It is this difference in the circadian rhythm between healthy cells and cancerous cells that Lévi wants to exploit. Genes that regulate drug detoxification and efflux mechanisms sit downstream of the clock genes, so their expression and activity have peaks and troughs throughout the day. If you can give a drug when these mechanisms are running high in healthy cells but low in tumorous cells, for instance, then toxic anticancer drugs will cause more damage to cancerous cells than healthy ones, and are more likely to be within the cell when the cell divides, the point at which traditional chemotherapeutics work.
From mouse to man
It is less than two years since Lévi moved to the University of Warwick from the French Institute of Health and Medical Research (INSERM) in Paris to set up a laboratory and work more closely with the systems biology team there, led by David Rand. Lévi’s office remains unfinished: textbooks dot otherwise bare shelves; piles of papers and folders clutter his desk and floor. The scrawlings on the whiteboard by his door give a clue about what he has been up to instead. He is refining his mathematical models to try to apply them to people, taking into account the potential of gene alterations in different tissues with different drugs. He wants to develop the same personalised treatment he has achieved with mice but in humans.
In an expansion of previous work that mapped varying peaks and troughs of effectiveness and tolerability of different cancer drugs in mice[3]
, in 2013 Lévi used mathematical modelling to try to tailor treatment to individual animals[4]
. He gave irinotecan, a drug used to treat bowel cancer, to mice from four genetic strains — optimal timing of the drug varied by up to eight hours depending on the animal’s sex and genetic background. After crunching the numbers, his model – which included information about the 24-hour expression of clock genes Rev-erbα and Bmal1 in liver and colon cells – could accurately predict the optimal time of drug tolerability, measured by weight loss, in any animal irrespective of its sex or genetic background. Timely administration led to a three-fold increase in tolerability.
For more than 15 years Lévi has treated patients in Paris with chronomodulated therapy, albeit with a slightly more low-tech equation. “Mouse plus 12 hours equals man,” he says with an apologetic grin. Since mice are nocturnal and people aren’t, he has been extrapolating the ideal treatment window from mice to man by adding 12 hours. It is a crude yet effective equation that has got him some interesting findings.
Between 1994 and 2006, Lévi conducted three randomised, multicentre trials of first-line fluorouracil and oxaliplatin with chronomodulated versus conventional delivery for metastatic colorectal cancer. He has been able to consistently reduce toxicity but efficacy results have been mixed. The first trial showed a benefit of chronotherapy in median survival but not median progression-free survival[5]
; the second showed a benefit in terms of tumour shrinkage but not survival[6]
; and the third showed no benefit in survival until a post-hoc analysis showed a three-month survival advantage of chronotherapy in men but not women[7]
. Findings from his 2012 meta-analysis of data for the 847 patients in all three trials substantiated the suggestion of a survival advantage in men but not women[8]
.
The difference between the sexes could be because toxicity from cancer drugs is about 25% higher in women than it is in men, Lévi suggests. When a drug is too toxic to a patient, their circadian rhythm is disturbed, thus negating any potential benefit of well-timed treatment[9]
.
Expanding the team
As a clinician-researcher, Lévi has been working on chronotherapy almost alone since the early 1990s, but he is being joined by a swell of basic scientists including Angela Relógio, a researcher at the Molecular Cancer Research Center and Institute for Theoretical Biology at Charité Medical University, Berlin.
Relógio, whose name means clock in her mother tongue Portuguese, was attracted to the field by the potential of its application, the seeming logicalness of the theory, and the fact that with new high-throughput technologies and molecular techniques, it is fertile scientific ground to plunder.
“What we’re trying to answer here is ‘do you have a clock change and then cancer or the other way around?’” she says. Because the biological clock reaches deep into a cell at a molecular level to affect the timing of processes such as cell division and DNA synthesis, she says, it makes sense that a disease such as cancer — caused by uncontrolled proliferation of cells — might be linked to a faulty clock. “From what we can see there seem to be links between a disrupted clock and cancer.”
From what we can see there seem to be links between a disrupted clock and cancer
Relógio is referring to observational findings that women who do night-shift work have a higher risk of cancer, but points out that the inherent confounding factors with observational studies weaken such findings[10]
. Analysis of her and her colleagues’ experimental and modelling data show that perturbations in the RAS expression system, a major driver of colorectal carcinogenesis, disrupt a cell’s circadian rhythm[11]
. Irradiated mice with their rhythm-dictating clock genes knocked out have a higher risk of cancer than wildtype ones[12]
.
A boon for Lévi’s cause, says Daniel Hochhauser, a medical oncologist at UCL Cancer Institute in London, is that scientists working with cancer drugs that differ in mode of action from conventional chemotherapeutics have found implications of chronotherapy for their findings. He cites a 2014 paper in which Yosef Yarden and colleagues, from the Weizmann Institute of Science in Israel, showed that downstream activation by the epidermal growth factor receptor (EGFR) gene — a target for antibody and small-molecule treatments in several cancers — is suppressed during night time in mice as a result of increased glucocorticoid secretion[13]
. There is reduced secretion of glucocorticoids during the resting phase and, by giving treatment at this time, there is increased effectiveness of EGFR inhibitors in mice with EGFR-driven tumours. In their paper, Yarden and colleagues note that “these findings support a circadian clock-based paradigm in cancer therapy” and explicitly call for further investigation in human studies.
“There’s still so much of the basic science missing,” says Relógio, referring to the challenges of converting experimental theory into demonstrable benefit in clinical trials. “In cancer a huge amount of things can go wrong, including the clock. The clock regulation of target genes is tissue dependent. We need to know more about the basic mechanisms and targets of the clock genes — what exactly are they regulating?”
We need to know more about the basic mechanisms and targets of the clock genes — what exactly are they regulating?
She is also conscious that the field needs more doctors. “I positioned my lab in the cancer centre here for a reason: to be close to doctors. Whenever I talk they think it’s really interesting but they say ‘you don’t really think you’re going to cure people with this do you?’”
Hochhauser can understand why. “It’s highly complex,” he says, stressing that he is not an expert in the field, and the fact that not many people are experts might be why the medical community has not historically placed much stock in the idea. “It’s difficult to find people working on chronotherapy because it’s kind of bizarre for many oncologists,” he says. “To think that the time that you give a treatment makes a difference is something that most clinicians will intrinsically think doesn’t sound credible.” But he adds that there might be something in it. “This is a very interesting area and one in which Professor Lévi is the undoubted pioneer.”
Relógio, too, hails Lévi as the doctor who has done the most to translate basic chronobiology into a treatment benefit for patients. His peers, though, have been less enthusiastic about his mission. “The concept is accepted scientifically,” says Lévi, “but let’s just say it’s not accepted with much enthusiasm in medical circles.”
The concept is accepted scientifically, but let’s just say it’s not accepted with much enthusiasm in medical circles
Other than the lack of prospective, randomised trials that show a survival benefit, Hochhauser points to other barriers to the wide-scale acceptance of chronotherapy. “We will need a better understanding of the biological rationale: how might timing of administration affect a drug’s half-life or metabolism, the toxicity of different drugs in different tissues, and what about the effects of complex combination therapies,” he says. “These are clearly areas Lévi and colleagues are exploring in depth and in which a systems biology approach will yield important results.”
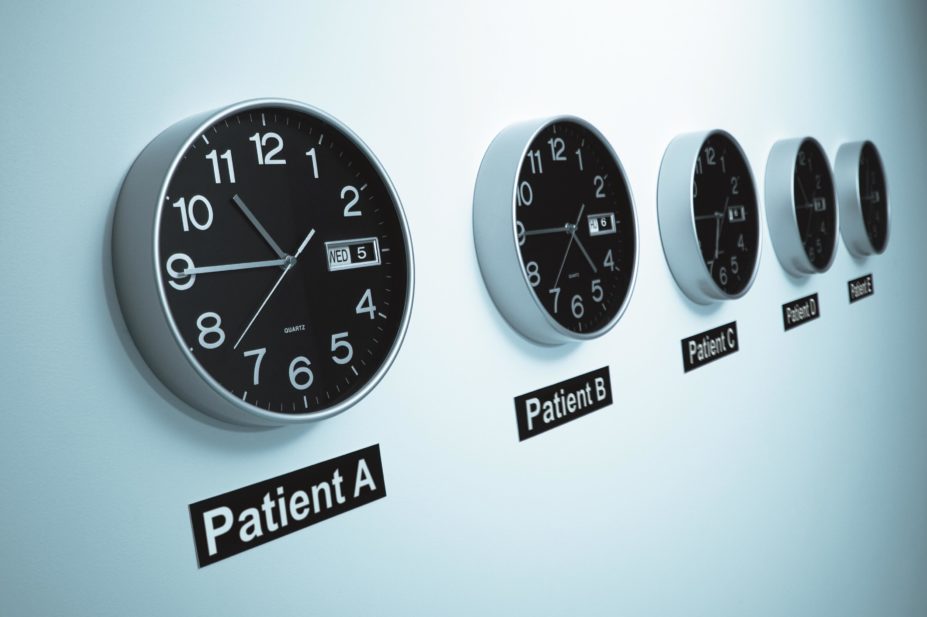
Logistically, too, there are obvious complications. “It would be a nightmare having to treat a patient at, say, two in the morning,” says Calum Polwart, lead pharmacist for cancer services at County Durham & Darlington NHS Foundation Trust, Durham. “But if it turns out to be the right thing to do for patients and would improve their outcomes, we would of course sit down and take a look properly.” Awkward administration can be overcome by using programmable pumps that could administer the drugs to patients in their homes. These pumps would be more expensive than existing ones.
“Mind you,” says Polwart, “the whole way we dose chemotherapy is fundamentally flawed — it’s not like it can’t be improved.” He explains that, because clinicians don’t fully understand each patient’s pharmacokinetics and pharmacodynamics, about 1% of patients die sooner than they would have. “We come pretty damn close to killing people,” he adds.
Manipulating molecular clocks
Marina Antoch, a molecular biologist at Roswell Park Cancer Institute in Buffalo, New York, is also concerned about the practical applications of chronotherapy in cancer. Like Lévi, though, she believes that the differing circadian rhythms in healthy and cancerous cells is a promising avenue of research to improve cancer treatment.
“To get around these practical problems,” she says, “our approach is to see if we can use small molecule drugs to reset the circadian rhythm of tumour cells to bring them within practical clinical treatment windows.” If she can identify molecules that can target only cancerous or healthy cells, there might be a way to manipulate molecular clocks so that clinicians don’t have to be at the whim of naturally occurring circadian schedules. This way, she says, the logistical complications and expense of timing treatment to a tumour’s time of high susceptibility, which could be in the middle of the night, will be negated.
Antoch is at the beginning of her research. “We’ve not yet moved into animal models,” she says, explaining that much of the research into understanding how small molecules can manipulate circadian rhythms has been done by basic scientists[14]
. Small molecules have broad ranging activity that might include interfering with important intracellular processes, such as the transcription of protein kinases. “We want to take that next step and to see if there are clinical applications of the technology,” she says. “I think it will take us about two to three years to identify and start testing in animal models. As far as when we’ll move into clinical testing, I don’t know. Translating into the clinic is not so easy.”
Hochhauser notes that, until recently, researchers investigating chronotherapy have been doing so molecularly blind. “Now that there is a better understanding of the rationale of gene interactions for chronotherapy, it might be possible to develop biomarkers to allow rational trial design. Success in these studies would stimulate more researchers to focus on this area.”
Unpacking circadian mechanisms

Source: Dara Mohammadi
Robert Dallmann, a circadian biologist and pharmacologist at the University of Warwick, says that for a long time the mechanisms behind circadian rhythms in cells were unknown
Over a walkway and into the building next to Lévi’s office sit two dishwasher-sized incubators in the team’s laboratory. Robert Dallmann, a circadian biologist and in vivo pharmacologist who left the University of Zurich to join Lévi in Warwick in 2015, explains that, by running tests on cancerous and healthy cells and tissue slices with bioluminescent reporter constructs, they can longitudinally measure expression in genes of interest at a granularity never before possible. Whereas researchers could previously measure expression of genes at only isolated time points, they can now track their activity in real time.
“For so long the mechanisms behind circadian rhythms in cells were a black box,” he says. “By doing molecular biology on them we can unpack it and start asking what does this all mean [in terms of] consequences for health and disease?”
Lévi is looking on proudly. “It’s a stepping stone towards personalised treatment,” he says of their efforts to feed this information into models and treatment algorithms that can be applicable for both traditional chemotherapeutics and new immunotherapies. “We have to design the proper methods to let us use these tools to their best potential and move forward very carefully.”
It’s a stepping stone towards personalised treatment
With chemistry and systems biology teams at Warwick they are embarking on a Cancer Research UK-funded project that Lévi is keeping tight-lipped about. “Let us get some data first and then we can say more,” he says, but divulges that it is an investigation of polymer-embedded chronotherapy. He has another trial starting in France in March 2016, which will assess the prognostic value of monitoring circadian rhythms and symptoms in patients with metastatic colorectal or lung cancer receiving chronotherapy.
“I really believe we are doing something good here and for the patients we are treating, otherwise I wouldn’t have kept on with it for 20 years,” says Lévi. “The problem is that it’s not only having the data but having it at the time when people are receptive to the idea.”
References
[1] Garcia-Sainz M & Halberg F. Mitotic rhythms in human cancer, reevaluated by electronic computer programs. Evidence for chronopathology. J Natl Cancer Inst 1966;37:279–292. doi: 10.1093/jnci/37.3.279
[2] Iurisci I, Filipski E, Reinhardt J et al. Improved tumor control through circadian clock induction by seliciclib, a cyclin-dependent kinase inhibitor. Cancer Res 2006;66:10720–10728. doi: 10.1158/0008-5472.CAN-06-2086
[3] Lévi F. From circadian rhythms to cancer chronotherapeutics. Chronobiol Int 2002;19:1–19. doi: 10.1081/CBI-120002676
[4] Li XM, Mohammad-Djafari A, Dumitru M et al. A circadian clock transcription model for the personalization of cancer chronotherapy. Cancer Research 2013;73:7176–7188. doi: 10.1158/0008-5472.CAN-13-1528
[5] Lévi FA, Zidani R, Vannetzel JM et al. Chronomodulated versus fixed-infusion-rate delivery of ambulatory chemotherapy with oxaliplatin, fluorouracil, and folinic acid (leucovorin) in patients with colorectal cancer metastases: a randomized multi-institutional trial. J Natl Cancer Inst 1994;86:1608–1617. doi: 10.1093/jnci/86.21.1608
[6] Lévi F, Zidani R & Misset JL. Randomised multicentre trial of chronotherapy with oxaliplatin, fluorouracil, and folinic acid in metastatic colorectal cancer. International Organization for Cancer Chronotherapy. The Lancet 1997;350:681–686. doi: 10.1016/S0140-6736(97)03358-8
[7] Giacchetti S, Bjarnason G, Garufi C et al. Phase III trial comparing 4-day chronomodulated therapy versus 2-day conventional delivery of fluorouracil, leucovorin, and oxaliplatin as first-line chemotherapy of metastatic colorectal cancer: the European Organisation for Research and Treatment of Cancer Chronotherapy Group. Journal of Clinical Oncology 2006;24:3562–3569. doi: 10.1200/JCO.2006.06.1440
[8] Giacchetti S, Dugué PA, Innominato PF et al. Sex moderates circadian chemotherapy effects on survival of patients with metastatic colorectal cancer: a meta-analysis. ARTBC International Chronotherapy Group. Annals of Oncology 2012;23:3110–3116. doi: 10.1093/annonc/mds148
[9] Innominato PF, Giacchetti S, Moreau T et al. Prediction of survival by neutropenia according to delivery schedule of oxaliplatin–5-Fluorouracil–leucovorin for metastatic colorectal cancer in a randomized international trial (EORTC 05963). Chronobiol Int 2011;28:586–600. doi: 10.3109/07420528.2011.597532
[10] Grundy A, Richardson H, Burstyn I et al. Increased risk of breast cancer associated with long-term shift work in Canada. Occup Environ Med 2013;70:831–838. doi: 10.1136/oemed-2013-101482
[11] Relógio A, Thomas P, Medina-Pérez P et al. Ras-mediated deregulation of the circadian clock in cancer. PLoS Genetics 2014;10:e1004338. doi: 10.1371/journal.pgen.1004338
[12] Fu L, Pelicano H, Liu J et al. The circadian gene Period2 plays an important role in tumor suppression and DNA damage response in vivo. Cell 2002;111:41–50. doi: 10.1016/S0092-8674(02)00961-3
[13] Lauriola M, Enuka Y, Zeisel A et al. Diurnal suppression of EGFR signalling by glucocorticoids and implications for tumour progression and treatment. Nature Communications 2014;5:5073. doi: 10.1038/ncomms6073
[14] He B & Chen Z. Molecular targets for small-molecule modulators of circadian clocks. Current Drug Metabolism 2016. doi: 10.2174/1389200217666160111124439


