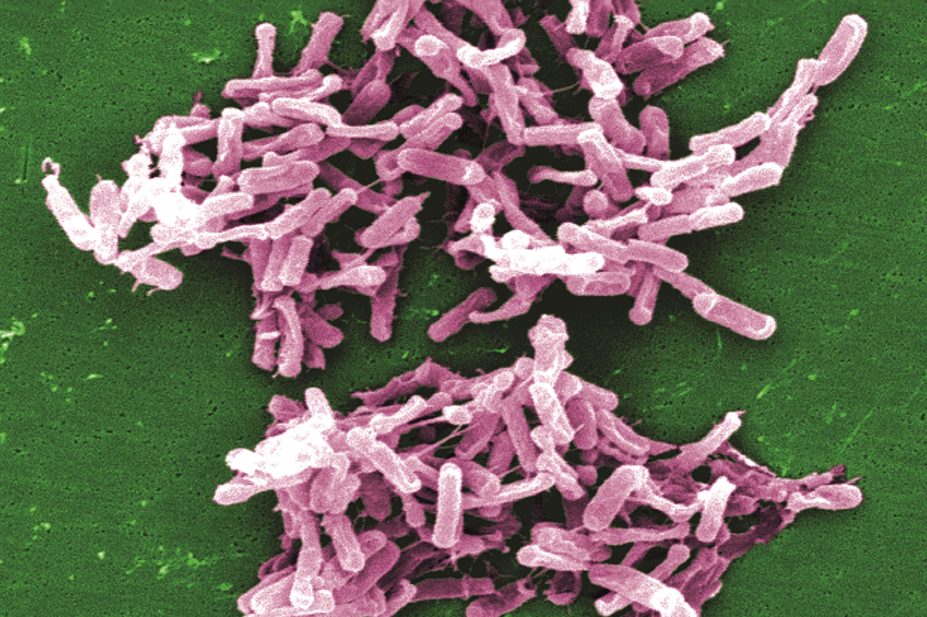
Janice Carr / CDC
The addition of a new human monoclonal antibody called bezlotoxumab to standard antibiotic treatment for Clostridium difficile infection can reduce the risk of a repeat infection, according to new research.
Two randomised, placebo-controlled trials, published in The New England Journal of Medicine
[1]
(online, 26 January 2017), involved 2,655 adults from 30 countries. All participants had primary or recurrent C. difficile infections and were receiving standard antibiotics (metronidazole, vancomycin or fidaxomicin).
The patients were randomly assigned to receive a single infusion of bezlotoxumab (10mg per kilogram of body weight); actoxumab (10mg per kg); bezlotoxumab plus actoxumab (10mg per kg each); or a placebo (saline).
Actoxumab and bezlotoxumab are human monoclonal antibodies that neutralise C. difficile toxins A and B, respectively.
After their C. difficile infection had resolved, patients were followed up for 12 weeks to see how many developed another C. difficile infection. In both trials, the rates of recurrent C. difficile infection were lower in people assigned to bezlotoxumab alone and to bezlotoxumab plus actoxumab compared with people in the placebo group.
The results showed that 17% and 16% of patients assigned to bezlotoxumab alone developed another C. difficile infection compared with 28% and 26% of those assigned to placebo, in each of the two trials. The addition of actoxumab did not improve efficacy.
The actoxumab alone arm of the trial was discontinued after a planned interim analysis because the rate of recurrent infection was found to be significantly higher in this group.

Source: Mark Wilcox
Lead author Mark Wilcox, professor of microbiology at the University of Leeds, says it is important to treat initial episodes of Clostridium difficile infection because each recurrence increases the chance of another episode
Lead author Mark Wilcox, professor of microbiology at the University of Leeds, says: “About one in four patients who have been treated with antibiotics for an initial C. difficile infection will go on to have a repeat infection. These repeat infections are more difficult to treat, have more severe outcomes for the patient, and are associated with more hospitalisations. [As a result,] it is important to treat the first episodes of C. difficile infection optimally, as each recurrence increases the chance of another episode even more.
“Fewer recurrent infections would mean less need to use antibiotics, fewer hospital admissions, reduced costs for the NHS and possibly a reduction in deaths.”
Wilcox adds: “The studies showed that bezlotoxumab was particularly effective in those patients with risk factors for poor outcome, including older age, immunocompromise, and severe infection.” As a result, he says doctors should consider which patients could best benefit from using bezlotoxumab.
John Bartlett, professor of medicine at Johns Hopkins University School of Medicine in Baltimore, Maryland, and the author of an accompanying editorial (ibid), says use of bezlotoxumab will need to be considered alongside alternative options, including new drugs and vaccines that are currently being evaluated in trials for the treatment and prevention of C. difficile infection.
“There are several important issues that are unresolved and need to be addressed to place this drug in perspective. Particularly important will be relative risk stratification and product cost,” he says.
One possible advantage of bezlotoxumab treatment, Bartlett adds, is that it provides “passive immunity to a microbial product” and is therefore not subject to the risk of antibiotic resistance.
“Nevertheless, it is noteworthy that C. difficile resistance to standard antibiotic therapy has not been problematic, despite extensive use of these agents,” he adds.
The US Food and Drug Administration approved bezlotoxumab (Zinplava; Merck) in October 2016, and in November 2016, the European Medicines Agency Committee for Medicinal Products for Human Use (CHMP) recommended that a marketing authorisation be granted.
The National Institute for Health and Care Excellence (NICE), England’s health technology assessment body, does not currently produce guidance on recurrent C. difficile infection, which occurs in approximately 20% of people within two weeks of treatment with either metronidazole or vancomycin.
However, NICE did publish a draft scope for a technology appraisal in November 2016 ahead of bezlotoxumab’s approval being granted in the UK. “Bezlotoxumab is a monoclonal antibody that targets C. difficile toxin B, suppressing symptoms to allow the body’s natural flora to replenish, preventing the need for further antibiotics cycles,” it says.
References
[1] Wilcox MH, Gerding DN, Poxton IR et al. Bezlotoxumab for prevention of recurrent Clostridium difficile infection. New England Journal of Medicine. doi: 10.1056/NEJMoa1602615


