Living Art Enterprises / Science Photo Library
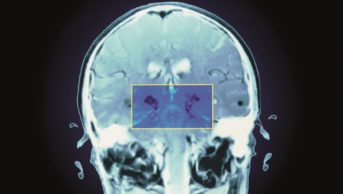
Researchers studying patients with chronic pain have shown they can predict those who will respond to placebo using functional magnetic resonance imaging (fMRI).
The team, from Northwestern University in Chicago, Illinois, found that around half of patients with chronic knee osteoarthritis pain experienced a strong analgesic response to placebo and the presence and magnitude of this response correlated with the level of connectivity in a region of the brain’s frontal lobe.
The researchers say the findings support the existence of an underlying biological basis for the placebo effect and could lead to ways to personalise pain treatments to patients based on brain scans, as well as improve results from clinical trials.
Apkar Apkarian, lead study author, says: “It may be useful as an actual treatment option since its effect size in responders is as large as existing pharmaceutical treatments.”
He adds that the information could also be used in trial settings to exclude subjects from the active treatment group. “If one could remove placebo responders from such trials then the real pharmacological effect can be detected in trials with a much smaller number of participants.”
The research, published in PloS Biology
[1]
(online, 27 October 2016), involved two studies.
The first was single-blinded and included 17 patients who received placebo for two weeks (but did not know whether they were having active treatment or not) followed by a two-week washout phase.
The researchers identified eight (47%) of the patients as placebo ‘responders’, defined as having at least a 20% reduction in knee pain as measured by a visual analogue scale after two weeks of treatment. They also found that ‘responders’ had robust responses to placebo, with a 54.3% mean decrease in their pain scores compared with no mean change among patients identified as ‘non-responders’.
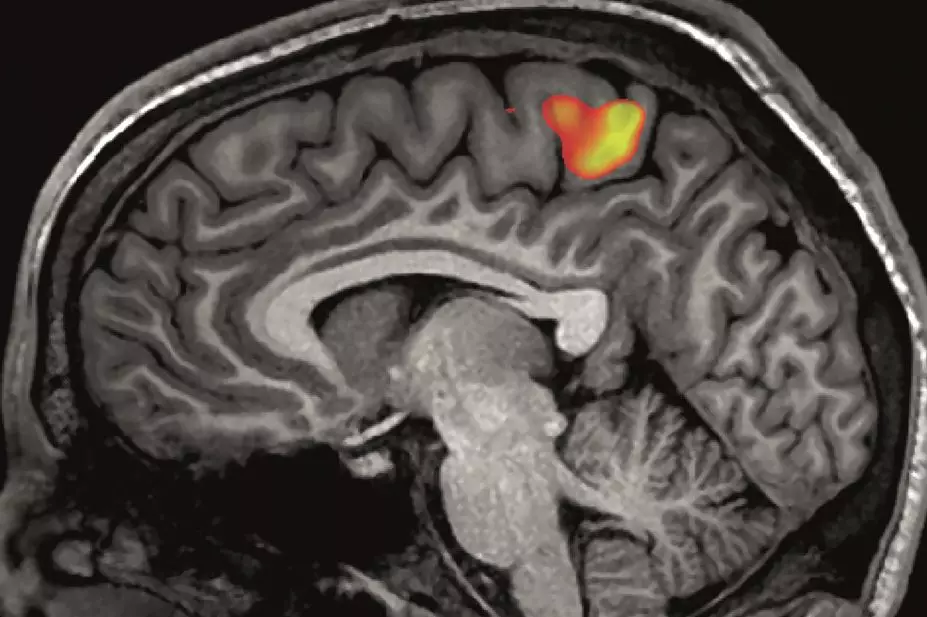
The team then looked at brain maps gathered before treatment began that used fMRI to count the number of connections within the brain. They identified four regions that had a significantly greater degree of connectivity among the placebo responders compared with non-responders, the highest of which was in a region called the right midfrontal gyrus (r-MFG).
The number of connections in the r-MFG predicted the magnitude of analgesia on both the visual analogue scale and an osteoarthritis-specific measure called the Western Ontario and McMaster Universities Osteoarthritis Index.
In the second study, the team validated their findings by carrying out a three-month double-blind clinical trial in which 39 patients were randomised to receive either the serotonin-norephinephrine reuptake inhibitor duloxetine or placebo. They found that r-MFG counts could differentiate responders from non-responders in the placebo arm with 95% accuracy. By contrast, r-MFG counts showed no association with duloxetine response.
Commenting on the second study, Luana Colloca, an associate professor at the University of Maryland, says that predicting placebo responses would be useful in tailoring the treatment of patients with pain.
“In real-world clinical settings, it would help to predict those patients who can benefit from a multidisciplinary approach to pain management and lower painkiller intakes,” she says.
However, she adds that this kind of research has some way to go before it can be applied like this. “This study is a great example of the potential high value of using brain scan to individualise pain management. However, the prospect of using brain scans to personalise pain management is still in its infancy,” she says.
Colloca adds that to be useful in a clinical setting, clinicians will need to be able to interpret fMRI data at an individual level. “Many brain imaging studies are currently based on group analyses — a scan of a single patient is not very informative. Also, any study on predictability of brain placebo effects deserves replication in larger trials enrolling patients with distinct chronic pain.”
References
[1] Tétreault P, Mansour A, Vachon-Presseau E et al. Brain connectivity predicts placebo response across chronic pain clinical trials. PloS Biology 2016;14:e1002570. doi: 10.1371/journal.pbio.1002570