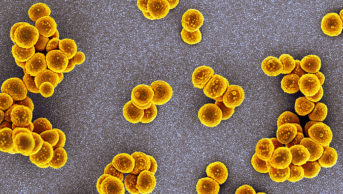
Wikimedia Commons
England’s chief medical officer Sally Davies has warned that if antibiotics lose their effectiveness it would spell “the end of modern medicine”.
Speaking at a United Nations Interagency Coordination Group (IACG) on Antimicrobial Resistance conference organised by the Wellcome Trust in partnership with the UK, Ghanaian and Thai governments in Berlin, Davies warned that unless action was taken on antimicrobial stewardship the world was facing a “post-antibiotic apocalypse”.
“I don’t want to say to my children that I didn’t do my best to protect them and their children,” Davies said.
She estimated that about one in three or one in four prescriptions in UK primary care were probably not needed.

Source: Courtesy, Conor Jamieson
Conor Jamieson, Royal Pharmaceutical Society clinical spokesman on antimicrobial resistance, and pharmacy team leader in antimicrobial therapy at Sandwell and West Birmingham NHS Trust, said that the government and the NHS were not taking the issue of antimicrobial resistance seriously enough
Conor Jamieson, RPS clinical spokesman on AMR and pharmacy team leader in antimicrobial therapy at Sandwell and West Birmingham NHS Trust said Davies was “absolutely right” that not enough was being done to tackle AMR.
“It is not being taken seriously enough at all levels in government and the NHS,” he said.
“What I see on wards every day is still a very high level of antibiotic prescribing.”
Jamieson also questioned whether medical and nursing staff, especially in secondary care, were being engaged and well enough informed about AMR.
The World Health Organization has said that each year around 480,000 people develop multi-drug resistant tuberculosis each year, with drug resistance starting to complicate the fight against HIV and malaria.
Davies warned that AMR was already here and “killing people”.
“This is a serious issue that is with us now, causing deaths,” she said.
“If it was anything else, people would be up in arms about it. But because it is hidden they just let it pass.
“Not to be able to effectively treat infections means that caesarean sections, hip replacements, modern surgery, is risky. Modern cancer treatment is risky and transplant medicine becomes a thing of the past,” she added.
In September 2017 the RPS launched a major new campaign calling on all pharmacists to play a greater role in safeguarding antibiotics and minimising the spread of antimicrobial resistance.
The Society is encouraging pharmacists to get involved in developing national and local action plans for antimicrobial stewardship (AMS) to ensure a ‘”robust evidence-based approach to the use of antibiotics”.
Royal College of GPs joint honorary secretary Jonathan Leach said there was a real risk of returning to a time when common illnesses killed people without further attempts to tackle AMR.
“We are increasingly using the policy of giving delayed prescriptions and that is becoming routine,” he said.
“I think pharmacists in surgeries are brilliant and can be a real help in flagging up patients who are on long-term antibiotics and by questioning antibiotic prescribing.”
RPS campaigns on antimicrobial stewardship
Antimicrobial stewardship has long been a policy and campaign focus of the Royal Pharmaceutical Society (RPS).
Responding to the UK Government’s Antimicrobial Resistance Strategy, published 13 September 2013, the RPS said that “Training of community pharmacists has the potential to reduce GP consultations by means of public education and symptomatic management of self-limiting infections”. In another response, to a 2014 NICE consultation on guidance for ‘Antimicrobial resistance: changing risk-related behaviours’ the Society said that the “use of minor ailment schemes whereby patients can receive symptomatic treatments for infections can decrease visits to a GP by 50% and reduce the number of prescribed antibiotics”.
In July 2014 the Society, together with the Royal College of General Practitioners (RCGP), the Royal College of Physicians (RCP), the Royal College of Nursing (RCN) and the UK Faculty of Public Health (FPH) published a Joint Statement on Antimicrobial Resistance. Among the recommendations of this statement was a call for antimicrobial prescribing data to be monitored, and for licensing requirements for new antimicrobials changed to include data on the minimum dosage required for clinical effectiveness.
In 2014, RPS Scotland collaborated with the Scottish Antimicrobial Prescribing Group (SAPG), Community Pharmacy Scotland and Pharmacy Voice to produce a European Antibiotic Awareness day resource pack for community pharmacists, which included a patient-directed self-care information leaflet for treating infectious ailments. The packs were distributed in November 2014.
Later that month, on European Antibiotic Awareness Day itself —18 November 2014 — RPS Scotland held a parliamentary reception and debate on antimicrobial resistance, sponsored by Jim Eadie MSP. The event led to a Scottish Parliamentary debate on the subject, held on 5 February 2015. Also on European Antibiotic Awareness Day, RPS Wales and the Royal College of General Practitioners (RCGP) held a lunchtime discussion with Welsh Assembly Members (AMs) on the use of antibiotics in primary care. During the summit, the two professional bodies called for Wales to commit to a public education campaign on the subject, and greater antimicrobial stewardship.
At the 2017 annual conference, the RPS launched its new GB-wide campaign on antimicrobial stewardship. The campaign aims to show how pharmacists are contributing to a targeted 50% reduction in inappropriate prescribing of antibiotics by 2020. As part of this campaign, the AMS portal— a hub for health professionals co-produced by the RPS and University College London — will be updated and relaunched.
Throughout all antimicrobial campaign and policy activity, the Antimicrobial Expert Advisory Group — chaired by antimicrobial pharmacist Harpal Dhillon —acts to advise the Society and shape policy on the subject.