Preclinical studies of interactions between selective serotonin reuptake inhibitors (SSRIs) and alcohol have mainly been acute experiments in healthy volunteers, using various psychological performance tests. The combination generally fails to impair function or produce other effects beyond those of alcohol alone.1,2 Alcohol use is common in depression,3 but its interaction with antidepressants in patients has been little studied except in problem drinkers. In a subgroup of these, alcohol problems seem to become worse.4,5
In our practices, we have repeatedly noted that some people experience a marked change in alcohol tolerance during treatment with SSRIs and related drugs. The consequences include disinhibition of violence or sexual behaviour, sometimes with profoundly impaired memory of the event.6,7 The same pattern appears across various SSRIs and venlafaxine, and in case reports from different countries,8 but clinicians do not routinely recognise or consider it. The mechanism is not clear, but the disinhibition from alcohol together with the stimulant effect of most SSRI and related antidepressants might lead to effects not seen with either alone. With this problem in mind, we examine the warnings for patients and prescribers in company information about prescribed SSRIs and related drugs.
Pathological intoxication
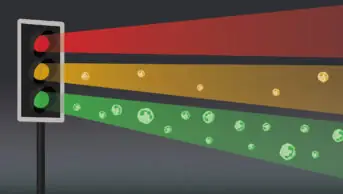
Pathological intoxication in a given individual refers to usual amounts of alcohol producing either a markedly exaggerated intoxication or qualitatively different intoxication, for example, with highly uncharacteristic disinhibition or violence
Our research
For venlafaxine, mirtazapine, bupropion, duloxetine and each of the SSRIs marketed in the UK, we examined the current summary of product characteristics (SPC) and patient information leaflet (PIL) and extracted all statements about interactions with alcohol, including warnings. We had in 2006–07 asked the UK medical directors of the main companies concerned for any information they had about possible interactions of their drug with alcohol, including experimental studies in volunteers, clinical studies, and case reports of suspected interactions.
Table 1 [currently not available] presents the SPC and PIL information. Almost all leaflets for clinicians and for patients stated in some way that alcohol should be avoided (SSRIs and venlafaxine) or used with caution (duloxetine). Most gave no specific reason for the advice. Some made the point generally. For example, the SPC for fluvoxamine states: “As with other psychotropic drugs patients should be advised to avoid alcohol.” But the corresponding PIL is more explicit: “Alcohol may interact and make you feel sleepy and unsteady.” Similarly, GSK’s PIL warned that alcohol use with paroxetine “may make symptoms or side effects worse”. Five of six UK companies marketing branded products (GSK, Lilly, Lundbeck, Pfizer and Wyeth) cited experimental data indicating that their drug(s) did not enhance the effects of alcohol, but still advised against the use of alcohol without explaining why.
Responses from companies to our further request for data on alcohol interactions varied greatly (Table 2, currently not available). Some came from a medical director or adviser, others from a pharmacovigilance executive. All were polite, but none had shown interest. Most sent a summary of one or more experimental studies in healthy volunteers, showing that acute doses of their drug and alcohol taken together had caused no greater mental or motor impairment than did alcohol alone. Several sent reports or summaries of published or unpublished clinical trials in alcoholics, testing whether their drug reduced alcohol intake or prevented relapse. None had found a positive benefit.
One company (GSK) sent an extensive literature search, but this was unfiltered and included many animal studies of doubtful relevance. No company sent a specific case report; most referred only to the number of cases in the Medicines and Healthcare products Regulatory Agency Yellow Card register. One claimed that the text of the reports was confidential. None of the international companies referred to cases reported outside the UK.
To drink or not to drink?
We found a general consistency across SPCs and PILs produced by makers of SSRIs and related antidepressants. Almost all discouraged alcohol use and, in something of a mixed message, cited evidence from healthy volunteer studies that their drug did not appear to interact with alcohol.
The warnings to avoid alcohol are thus unsupported by specific evidence. They appear weak and unconvincing for both prescribers and patients. This may explain why many patients do not take the warning seriously.
We have described a syndrome of pathological intoxication, often with serious consequences, in patients prescribed an SSRI or related drug.6–8
It is striking that often only modest or usual amounts of alcohol are involved, and that memory is impaired in roughly half of such cases. The problem is not rare, but it is often not recognised. That may relate both to the well known under-reporting of adverse events, and the possibility that regulators have not routinely considered such effects by drug class. For example, the MHRA online database includes 129 reports categorised as “interaction with alcohol” of SSRI and related drugs, but these are not considered as a group. The reports are aggregated by individual drug name and relationships between drugs are not visible.9
SPCs and PILs need to be strengthened to warn prescribers and patients clearly about the possibility of pathological alcohol intoxication during treatment with SSRIs and related drugs. This should improve prescribing choices and facilitate detection and study of the problem.
References
- Allen D, Lader M. Interactions of alcohol with amitriptyline, fluoxetine and placebo in normal subjects. International Clinical Psychopharmacology 1989;4(Suppl 1):7–14.
- Schaffler K. Study on performance and alcohol interaction with the antidepressant fluoxetine. International Clinical Psychopharmacology 1989;4(Suppl 1):15–20.
- Davis LL, Rush JA, Wisniewski SR, Rice K, Cassano P, Jewell ME et al. Substance use disorder comorbidity in major depressive disorder: an exploratory analysis of the Sequenced Treatment Alternatives to Relieve Depression cohort. Comprehensive Psychiatry 2005;46:81–9.
- Chick J, Aschauer H, Hornik K. Efficacy of fluvoxamine in preventing relapse in alcohol dependence: a one-year, double-blind, placebo-controlled multicentre study with analysis by typology. Drug and Alcohol Dependence 2004;74:61–70.
- Lingford-Hughes AR, Welch S, Nutt DJ. Evidence-based guidelines for the pharmacological management of substance misuse, addiction and comorbidity: recommendations from the British Association for Psychopharmacology. Journal of Psychopharmacology 2004;18:293–335.
- Chandler P, Herxheimer A. Unexpected aggressive behaviour: interaction of bupropion and alcohol. International Journal of Risk and Safety in Medicine 2011;23:133–7.
- Herxheimer A. British diplomat cleared of drunk flying charges: paroxetine was involved. International Journal of Risk and Safety in Medicine 2007;19:35–40.
- Menkes DB, Herxheimer A. Provocation by alcohol of violence as a side-effect of antidepressants. Drug Safety 2009;32:948–9.
- Download Drug Analysis Prints (DAPs). London: Medicines and Healthcare products Regulatory Agency (MHRA); 2011. Available at: www.mhra.gov.uk (accessed 30 November 2011).