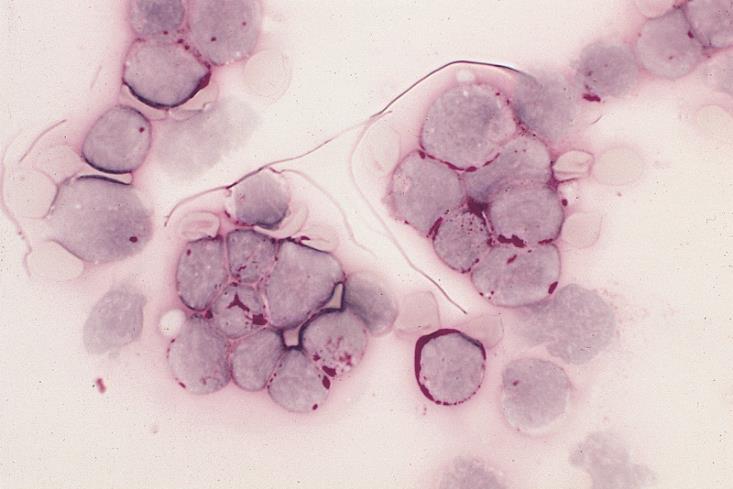
Wikimedia Commons / The Armed Forces Institute of Pathology
Patients with acute lymphoblastic leukaemia (ALL) that has relapsed after treatment are almost four times as likely to go into remission and have a potentially curative stem cell transplant following treatment with a new antibody drug conjugate.
In the phase III trial, sponsored by Pfizer, 326 patients with relapsed or refractory ALL, an aggressive cancer that starts in the bone marrow and has a high relapse rate, were randomly assigned to receive either inotuzumab ozogamicin or standard intensive chemotherapy.
With standard treatments, the chance of achieving remission is low once patients have relapsed, but the researchers found that 80.7% of relapsed patients given inotuzumab ozogamicin went into complete remission compared with 29.4% treated with standard therapy (P<0.001). Some 41% of patients in the inotuzumab ozogamicin group went on to have an allogenic stem cell transplant, compared with 11% of patients given standard chemotherapy (P<0.001).
Even after transplant, ALL can come back again, but the results show that it took longer on average for the disease to return in the inotuzumab ozogamicin group: 5.0 months compared with 1.8 months in the standard treatment group.
Reporting the results in The
New England Journal of Medicine
[1]
(online, 12 June 2016), lead author Hagop Kantarjian, from the Universtiy of Texas MD Anderson Cancer Center, says: “Given that stem cell transplant is considered the only curative treatment option [for ALL], the ability of inotuzumab ozogamicin to increase the number of patients able to bridge to transplant is encouraging.”
Median survival was 7.7 months in the inotuzumab ozogamicin group compared with 6.7 months in the standard treatment group. And in an analysis of overall survival at two years, 23% of patients in the inotuzumab ozogamicin group had survived compared with 10% in the standard therapy group (P=0.04).
Inotuzumab ozogamicin is a novel type of therapy that is increasingly being used to treat cancer. It links a targeted monoclonal antibody to a toxic drug. The monoclonal antibody in inotuzumab ozogamicin targets a glycoprotein on the surface of cells called CD22, which is expressed in 90% of patients with B-cell ALL. Once the monoclonal antibody reaches the targeted cells it is internalised and releases calicheamicin, a toxic drug that kills the cell.
Peter Johnson, chief clinician at Cancer Research UK, who was not involved in the study, says: “Acute lymphoblastic leukaemia that comes back after chemotherapy is difficult to treat. Bone marrow transplants are the best hope for these patients, but the leukaemia must be controlled first before having a transplant.”
He adds that “the good news is this treatment may be one way to help patients into remission ready for a transplant”.
“Although it’s not a cure on its own, it could be a useful pre-treatment that helps more leukaemia patients have life-saving bone marrow transplants.”
The most serious side effect observed in the clinical trial was veno-occlusive liver disease, which occurred in 11% of patients in the inotuzumab ozogamicin group compared with 1% in the standard treatment group.
References
[1] Kantarjian, HM, DeAngelo, DJ, Stelljas, M et al. Inotuzumab Ozogamicin versus Standard Therapy for Acute Lymphoblastic Leukemia. The New England Journal of Medicine 2016. doi: 10.1056/NEJMoa1509277