Shutterstock.om
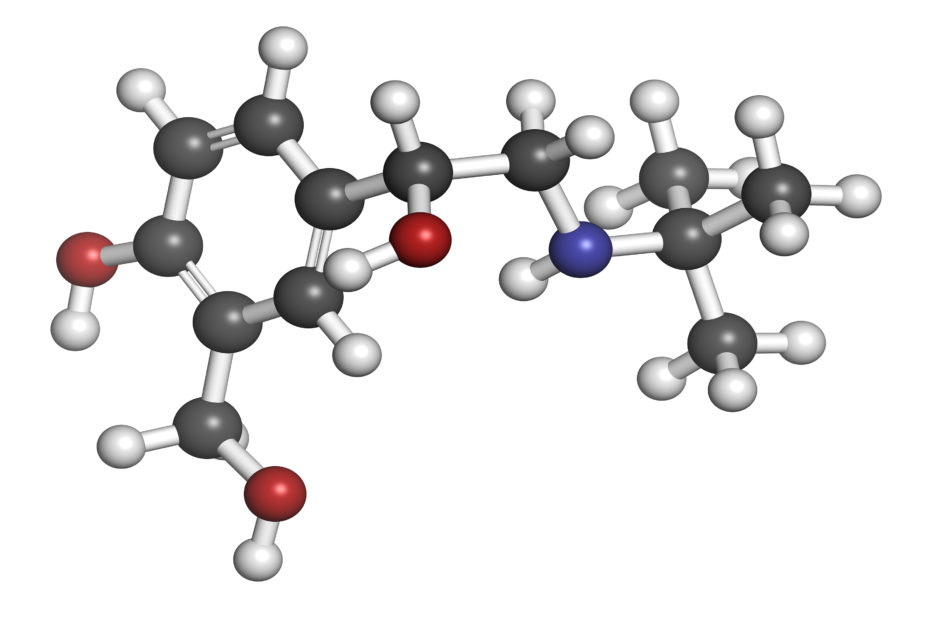
Research has found that the asthma drug salbutamol is associated with a reduction in the risk of Parkinson’s disease (PD).
The
Science study identified a role for the beta-2 adrenergic receptor (ß2AR) in the regulation of α-synuclein, a protein that has been implicated in the development of PD.
And the researchers used national prescribing data from Norway to show that people who took salbutamol, which interacts with this receptor, were approximately a third less likely to receive a PD diagnosis than others.
They say it should now be explored if the compound has an effect in people already living with the disease.
“These medicines have never been studied in relation to Parkinson’s disease,” said study author Trond Riise from the University of Bergen.
“Our discoveries may be the start of a totally new possible treatment for this serious disease.”
The team screened over 1000 compounds to identify those that had an effect on the expression of the α-synuclein gene SNCA, which yielded several ß2AR agonists including clenbuterol and salbutamol as potential candidates.
Then, using a database of 4.6m people living in Norway since 2004, they showed that salbutamol was associated with a significantly reduced risk of PD (rate ratio: 0.66) during 11 years of follow-up. And, by contrast, propanolol, the most commonly used ß2AR antagonist was associated with a significantly increased risk of the disease (rate ratio: 2.20).
Previous research has looked at pharmacological approaches to enhance the clearance of α-synuclein or prevent its transformation into toxic species in the brain. But the authors say their approach is different in seeking to reduce the transcription of the protein’s gene and to prevent or stall disease progression.
Future research, including clinical trials, will be needed to establish if this translates to practice in people with PD, they conclude.
References

