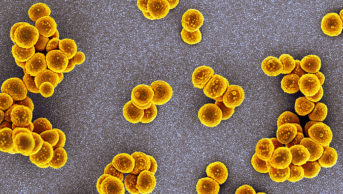
MBI / Alamy Stock Photo
GPs who prescribe the most antibiotics reduce the amount they prescribe by avoiding unnecessary prescriptions if they are sent feedback benchmarking their prescribing levels against those of their peers, a study[1]
has found.
Advising GPs with the highest levels of antibiotic prescribing levels was an approach recommended by the National Institute of Care and Excellence in its antibiotic stewardship guidelines in 2015. The study, published in The Lancet (online, 18 February 2016) and carried out in collaboration with England’s health authorities, found that this advice process cut antibiotic dispensing by 3.3% over six months.
In September 2014, the researchers identified 1,581 GP practices in England with antibiotic prescribing rates in the top 20% for their area. The practices were then randomly assigned to either receive a letter from the chief medical officer Dame Sally Davies highlighting their high prescribing rate, or to receive no communication.
The letter told GPs that “80% of practices in their local area prescribe fewer antibiotics per head than yours” and suggested three ways to make sure prescriptions for antibiotics were necessary. These included: giving patients advice on self-care; offering a delayed prescription; and talking to other prescribers in their practice to ensure they were prescribing appropriately.
GPs who received the letter prescribed 3.3% fewer antibiotics over six months from October 2014 to March 2015 than those who received no communication; the rate of prescribing was 127.0 items in the intervention group compared with 131.3 in the control group — 4·3 items per 1,000 people lower.
Overall, the 791 GP practices in the intervention group dispensed 73,406 fewer antibiotic items. The cost of printing and mailing letters to the 3,227 GPs in those practices was £4,335, equivalent to £0.06 per prescription prevented. The researchers calculated that the intervention saved £92,356 in direct prescribing costs.
Between 2000 and 2014, UK primary care antibiotic use increased by 46%, and the UK government[2]
set a goal in 2013 to reduce antibiotic prescribing in primary care by 4% by 2018, as part of efforts to tackle growing antimicrobial resistance.
Michael Hallsworth, from the Behavioural Insights Team, a company part owned by the UK government, led the study and said that this type of behavioural intervention could help achieve the 2018 target. “This simple intervention could reduce England’s antibiotic prescribing by 0.85% overall, despite costing just six pence per prescription saved,” he says.
“This kind of feedback could also be provided for many other kinds of drugs, and by anyone who is interested in doing so, since all this information is publicly available online.”
Maureen Baker, chair of the Royal College of General Practitioners, said that while GPs are open to feedback and welcome a reflective approach to prescribing, it was important that this approach is combined with work to make the public realise that prescribing antibiotics is not always the answer to treating minor, self-limiting illness.
“GPs already undertake regular prescribing reviews to see what they can do differently in the best interests of their patients. Reminder letters could be seen as an extension to this — or a prompt — but it’s important that doctors who receive letters don’t feel overly-criticised as a result,” she says.
“There is nothing to say that doctors who prescribe the most antibiotics are doing so inappropriately; some doctors will prescribe more than others simply as a result of the demographics of their patients.”
References
[1] Hallsworth M, Chadborn T, Sallis A et al. Provision of social norm feedback to high prescribers of antibiotics in general practice: a pragmatic national randomised controlled trial. The Lancet 2016;S0140-6736(16):00215-4. doi: 10.1016/S0140-6736(16)00215-4
[2] Department of Health and Department for Environment, Food, and Rural Affairs. UK 5 year antimicrobial resistance (AMR) strategy 2013 to 2018.