Dr P Marazzi / Science Photo Library
The worldwide prevalence of obesity has continued to dramatically increase over the past few decades [1],[2],[3]
. More than 2 billion people are considered as being overweight globally, of whom 600 million are considered obese, defined as a body mass index (BMI) of ≥30 kg/m2[1],[2]
. Obesity is a complex chronic multisystem condition with physiological, psychological and social implications. It is described as abnormal, excessive fat accumulation and contributes to a significant increase in mortality [1],[4],[5]
. In the UK, rates doubled between 1993 and 2011[6]
and the estimated prevalence of being overweight or obese is 62.1%[7]
. In comparison, the United States has an estimated prevalence of up to 75%, with 6.3% being morbidly obese (BMI of ≥50kg/m2)[1],[2],[8]
(see ‘Graph 1: Prevalence of obesity worldwide’).
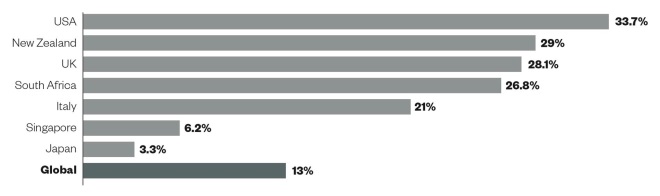
Graph 1: Prevalence of obesity worldwide
Source: World Health Organization
The prevalence of obesity in the United States, New Zealand, UK and South Africa are well above the global prevalence of 13%. Singapore and Japan have a much lower prevalence of obesity in comparison.
The UK societal cost of treating obesity and associated comorbidities is estimated to reach £7bn per year, with £1bn per year attributed to health service costs[9]
. Further calculations have predicted that by 2050, obesity will add £5.5bn to the total annual cost of the NHS[9],[10]
. In response, there have been efforts to educate and promote lifestyle and medical therapies, including exercise regimens, dietary advice and lipase inhibitors such as Orlistat (tetrahydrolipstatin)[1]
. However, results are modest and sustained weight loss is rarely achieved[3],[11],[12],[13]
.
Consequently, bariatric surgery is increasingly popular and techniques have advanced since the first operations were described in the 1950s. Complication rates in the UK are approximately 2.9%[14]
, while global mortality rates are around 0.07% and surgery is often associated with a short length of stay in hospital (mean 2.7 days)[12],[15]
. The National Institute for Health and Care Excellence (NICE) guidelines currently offer bariatric surgery to people with a BMI of ≥40kg/m2 or 35–40kg/m2, plus one medical condition that may be improved with weight loss[16]
(see ‘Box 1: The National Institute for Health and Care Excellence criteria for consideration of bariatric surgery’). However, there is a significant mismatch between eligible patients (approximately 260,000 in the UK) and uptake of surgery, which may be on account of a lack of adequate resources and a lack of understanding of the criteria for bariatric surgery[16],[17]
.
Box 1: The National Institute for Health and Care Excellence (NICE) criteria for consideration of bariatric surgery
Criteria:
- BMI of ≥40 kg/m2 OR
- BMI of 35-40 kg/m2 and another significant disease:
- Recent onset type 2 diabetes
- Hypertension
- Sleep apnoea
- Benign intracranial hypertension
AND
- Appropriate non-surgical measures have been trialled but clinically beneficial weight loss has not be achieved or sustained for ≥6 months;
- Patient is committed to long-term follow-up;
- Must be managed in a psychologically led multidisciplinary bariatric service (tier 3).
Source: National Institute for Health and Care Excellence
[16]
In the UK, 16,956 bariatric surgical procedures were carried out between 2011 and 2013, on patients with an average BMI of 48.8kg/m3. In contrast, 179,000 operations were carried out in the United States in 2013 alone[12]
. The majority of patients having bariatric surgery in the UK are aged 45–54 years. Worldwide, more adolescents are now undergoing surgery on account of an increasing prevalence of significant comorbidities and an increased prevalence of adolescents who are “super-obese” (i.e. BMI of ≥45)[3],[12]
. There is also a global trend towards operating on higher risk individuals with established disease or end-organ damage[3]
. This is because surgical management can increase lifespan[18]
and lead to improvement in a number of conditions, such as diabetes and hyperlipidaemia[3],[12],[13],[19]
(see ‘Graph 2: Improvement or resolution of associated conditions following bariatric surgery’) as well as significant weight loss (see ‘Graph 3: Loss of excess body weight (EBW) after bariatric surgery’)[3]
. Consequently, bariatric surgery is cost-effective in the developed world on account of reductions in obesity-related conditions and an increase in quality of life[11],[12]
.
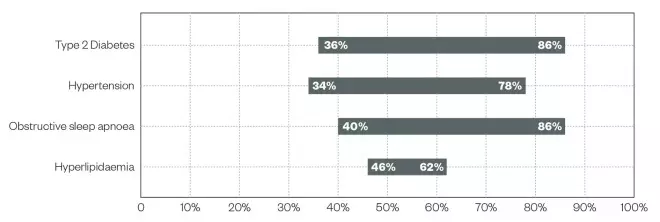
Graph 2: Improvement or resolution of associated conditions following bariatric surgery
Source: The British Obesity and Metabolic Surgery Society[3]
; American Society for Metabolic and Bariatric Surgery[12]
; Siostrom et al. NEJM 2004;351:2683-2693[13]
; Puzziferri et al. JAMA 2014;312:934-942[19]
Currently there is a global trend towards operating on higher risk individuals with established disease or end-organ damage. This is because surgical management can increase lifespan and lead to improvement in a number of conditions, such as diabetes and hyperlipidaemia
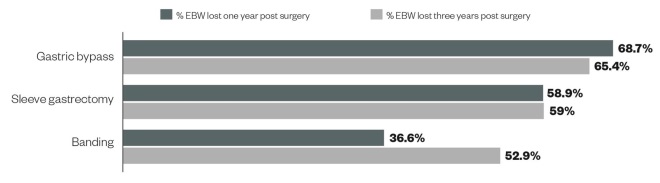
Graph 3: Loss of excess body weight (EBW) after bariatric surgery
Source: World Health Organization
Surgical management can lead to significant weight loss and reduction in excess body weight (EBW). Gastric bypass is associated with the highest percentage of EBW lost at one year and three years post-surgery
Bariatric surgery, in its various forms, affects specific sites involved in drug absorption and metabolism, potentially affecting pharmacological management in individuals who have undergone surgery.
This article will discuss types of bariatric surgery, the impact on drug pharmacokinetics and specific recommendations for drug regimens following bariatric surgery.
Types of bariatric surgery
Bariatric surgery was traditionally categorised into restrictive, malabsorptive and combined types. More recent understanding that these surgical procedures alter hormonal regulation of metabolism has superseded this categorisation (see ‘Table 1: Proposed mechanism of bariatric surgery’)[20]
,[21],[22],[23],[24],[25]
.
| Table 1: Proposed mechanism of bariatric surgery . | |||||
|---|---|---|---|---|---|
| Hormone | Site of release | Action | Gastric band | Roux-en-Y gastric bypass | Sleeve gastrectomy |
| Glucagon-like Peptide 1 (GLP1) | L-cells (distal ileum and colon) | Increased satiety, increases beta-cell mass, slows gastric emptying | No clear effect observed[20] | Increased[21],[22] | Increased[21],[22] |
| Glucagon-like Peptide 2 (GLP2) | L-cells (distal ileum and colon) | Increases mucosal cells and crypt cell mass. Increases cells releasing GLP1 | No clear effect observed[20] | Increased[23] | No clear effect observed[21] |
| Peptide YY | L-cells (distal ileum and colon) | Increased satiety, inhibits intestinal motility, slows gastric emptying | No clear effect observed[20] | Increased[21],[23] | Increased[21],[22] |
| Oxyntomodulin | L-cells (distal ileum and colon) | Inhibits intestinal motility | No clear effect observed[20] | Increased[24] | No clear effect observed [21] |
| Ghrelin | Stomach, duodenum, jejunum and ileum | Stimulates appetite | No clear effect observed[20] | Decreased[21],[22] | Decreased[21],[22] |
| Vagus nerve | Afferent fibres affect L-cells | Stimulates appetite, hormonal action via ghrelin | No clear effect observed[20] | Weight loss combined with vagotomy[25] | Weight loss combined with vagotomy[25] |
Surgical procedures comprise those that decrease stomach volume or that utilise a bypass of part of the gastrointestinal tract. These include adjustable gastric banding (AGB), sleeve gastrectomy (SG), Roux-en-Y gastric bypass (RYGB), the bilio-pancreatic bypass/duodenal switch procedure and vertical banded gastroplasty (see ‘Figure 1: Types of bariatric surgical procedures’).
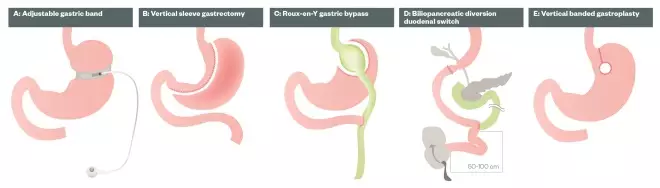
Figure 1: Types of bariatric surgical procedures
A. Adjustable gastric band: A laprascopic adjustable gastric band is an inflatable device that is placed around the upper part of the stomach, with the aim of slowing consumption of food, reducing the amount of food consumed.
B. Vertical sleeve gastrectomy: The stomach is reduced to around 25% of its original size by surgical removal of a large portion of the stomach along the greater curvature.
C. Roux-en-Y gastric bypass: The size of the stomach is reduced to a small pouch, around the size of an egg. A large section of the stomach is stapled off and the pouch is attached to the small intestine, bypassing much of the stomach and the upper part of the small intestine.
D. Biliopancreatic diversion with duodenal switch: The stomach is divided, removing the outer margin, leaving a sleeve of stomach with the pylorus and duodenum at the end. The duodenum is divided so that pancreatic and bile drainage is bypassed. The near end of the alimentary limb is attached to the beginning of the duodenum and a common limb is created.
E. Vertical banded gastroplasty: Also known as stomach stapling, a band and staples are used to create a small stomach pouch. A 1cm hole at the bottom of the pouch allows the contents to flow into the remainder of the stomach, and then pass into the gastrointestinal tract.
AGB involves application of a synthetic band just distal to the gastro-oesophageal junction, creating a gastric pouch with a small outlet (≈ 1cm diameter). The band can be inflated or deflated via an external port.
In SG, the stomach is stapled vertically, essentially removing the greater curvature and preserving the pylorus and antrum.
In RYGB, the stomach is reduced to approximately the size of a golf ball and the outlet measures around 1cm in diameter. A section of small intestine between the jejunum and ileum is divided and the proximal end of the shortened distal ileum (‘Roux’ limb) is attached to the new gastric pouch, bypassing the duodenum and jejunum, a primary site for absorption of nutrients and medications. The bilio-pancreatic limb of the jejunum, carrying biliary and gastric secretions, is then reconnected to the small intestine distal to the gastro-jejunal anastomosis (80–120cm) creating a ‘common limb,’ where food contents and digestive enzymes mix.
The bilio-pancreatic bypass/duodenal switch is a variation of RYGB where a longer length of the small intestine is bypassed. This leads to profound weight loss but has an increased operative time (usually performed as a two-part procedure), post-operative risks and higher malnutrition rate. Therefore, it is usually reserved for the severely obese with a BMI of ≥50-60.
The now virtually unused vertical banded gastroplasty involves partitioning of the stomach with staples and then use of a band to create a small gastric pouch. Although not routinely performed, patients who have had this procedure will continue to present to health services.
In the United States and the UK, RYGB and SG represent the majority of bariatric procedures and more than 90% are performed laparoscopically[3],[12]
.
Bariatric surgery is cost-effective and safe[3],[10],[11]
[12
]
,[17]
but it introduces concern about nutrient delivery and altered drug pharmacokinetics. There have been no prospective, randomised studies to date looking at drug pharmacokinetics in the post-bariatric surgery population,[26],[27]
however, in vitro studies and case series have provided some suggestion of drug-specific alterations in drug pharmacokinetics.
Absorption and bioavailability
Nearly all nutrient and oral absorption occurs in the small intestine, which normally has an absorptive surface area of 250m2. Important considerations here include drug specific factors (i.e. ionisation, lipophilicity, stability, dissolution properties) and patient factors (i.e. gastric pH, gastric emptying, area of mucosal exposure and contact with transporter systems). The type of surgery has an impact, with bypass procedures theoretically more likely to affect overall absorption, on account of loss of mucosal exposure and reduced bile-salt mixing[26],[27]
.
It is important to remember drug dosage and regimens are developed in trials involving participants with ‘normal’ gastrointestinal anatomy. Therefore, bariatric patients may exhibit altered responses to standard medications and doses[26],[27],[28],[29],[30],[31],[32],[33],[34],[35],[36],[37],[38],[39],[40],[41],[42],[43],[44],[45],[46],[47],[48],[49]
(see ‘Table 2: Medications with specific advice following bariatric surgery’).
| Table 2: Table of medications with specific advice following bariatric surgery | |||
|---|---|---|---|
| Medication | Evidence for altered absorption? | Possible action | Alternative preparations |
| Amitriptyline | Possibly reduced (in vitro). [26],[27],[28] | Monitor levels closely. Lipophillic drug | Sugar-free liquid (10mg/5ml or 25mg/5ml concentrations)[29] |
| Atazanavir | No significant change observed[30] | Monitor CD4 and viral load closely | Oral solution available[29] |
| Atorvastatin | Possibly increased[31],[32] | Monitor cholesterol | Lipitor (Pfizer) brand tablets disperse within 2–5 minutes when placed in 10ml of water, to produce a very fine milky, white dispersion that does not settle quickly. Most preparations are film coated. A chewable tablet version from Pfizer is also available[33] |
| Bupropion | Reduced (in vitro)[28] | Close psychiatric monitoring | No alternative |
| Citalopram | No significant change/ possibly reduced[28],[34] | Close psychiatric monitoring | Citalopram oral drops (40mg/ml). Unlicensed intravenous Citalopram 20mg/0.5ml can be sourced[35] |
| Darunavir | No significant change observed[30] | Monitor CD4 and viral load closely | Oral suspension (100mg/ml concentration)[29] |
| Digoxin | No significant change[26],[27] | Monitor levels closely. | Elixir 50µg/ml[36] |
| Enalapril | Unclear[37] | Monitor blood pressure. Requirements may fall | Enalapril 1mg/ml solution. Tablets can be crushed and dispersed in water[29] |
| Fluoxetine | Reduced (in vitro)[28],[38] | Close psychiatric monitoring | Liquid 20mg/5ml (Lilly brand does not contain sorbitol. Prozit brand contains ethanol and 3g/5ml sucrose)[38] |
| Ketoconazole | Possibly reduced[37] | Needs acidic medium for absorption. Consider an alternative. | No alternative. Other antifungals are available in parenteral formulations[29] |
| Lamotrigine | Possibly reduced[39] | Monitor closely | Dispersible tablets in 2mg, 5mg, 25mg and 100mg available[39] |
| Levothyroxine | Unclear[31] | Monitor closely. Regular thyroid function testing | Tablets disperse in water or can be crushed. Oral solutions of 25µg/5ml, 50µg/5ml and 100µg/5ml dependent upon manufacturer[40] |
| Lithium carbonate | Increased[26],[28] | Close psychiatric monitoring | Oral solution as Lithium Citrate 520mg/5ml (Contains 96% ethanol 0.26 ml/5 ml)[41] |
| Metformin | Possibly increased [31],[37],[42] | Monitor blood glucose closely. Requirements may fall | Oral solution 500mg/5ml (does not contain sorbitol)[21],[22],[23]. Powder for oral solution (500mg and 1000mg). Modified release tablets cannot be crusehd and are not suitable for enteral tube administration[43] |
| Metoprolol | No significant change [37],[44] | Monitor blood pressure. Requirements may fall | Tablets can be readily crushed but not readily disperse in water[15]. Manufacturer’s special oral solutions available in 12.5mg/5ml, 50mg/5ml and 10mg/5ml[44] |
| Morphine | No significant change[31] | Monitor closely | Oral solutions 10mg/5ml or concentrated 20mg/ml. Modified release granules available in 20mg, 30mg, 60mg, 100mg or 200mg[29] |
| Mycophenalate | Reduced[31],[45] | Monitor closely | Oral suspension 1g/5ml and intravenous 500mg vials available[45] |
| Olanzapine | Reduced[28],[37],[46] | Close psychiatric monitoring. Monitor levels regularly | Orodispersible tablets available in 2.5mg, 5mg, 7.5mg, 10mg, 15mg and 20mg[29],[46] |
| Omeprazole | No significant change[31] | Monitor symptoms closely | Dispersible tablets available in 10mg, 20mg and 40mg. Intravenous injection available in 40mg vials[47] |
| Paracetamol | No significant change[31],[37] | Monitor symptoms closely | Soluble 500mg tablets, Oral suspension 125mg/5ml and 250mg/5ml, Infusions available in 500mg and 1g[29] |
| Paroxetine | Reduced (in vitro)[28],[48] | Close psychiatric monitoring | Liquid 10mg/5ml available[48] |
| Phenytoin | Reduced[26],[27] | Monitor levels closely | Oral suspension (30mg/5ml)[29] |
| Ritonavir | No significant change observed[30] | Monitor CD4 and viral load closely | Oral solution (80mg/ml)[29] |
| Sertraline | Reduced (in vitro) [26],[28], [31] | Close psychiatric monitoring | Lustral tablets may be crushed, suspended in sterile water and administered using a suitable syringe. Oral suspension 50mg/5ml as manufacturer’s special can be obtained[33] |
| Simvastatin | Unclear [26],[37] | Monitor cholesterol | Oral suspension available from Rosemont (20mg/5ml and 40mg/5ml). Tablets can be crushed and dispersed in water. However, film coated tablets are not suitable for enteral administration[43] |
| Tacrolimus | Reduced[27],[31] | Monitor levels closely | Concentrate for injection 5mg/ml available. Granules for oral suspension available in 0.2mg and 1mg, which are suitable for nasogastric tube administration[49] |
| Tenofovir | No significant change observed[30] | Monitor CD4 and viral load closely | Available as a powder[29] |
Gastric pH
In the first instance, drug breakdown and solubility is affected by gastric pH. Drugs more soluble at an acidic pH are absorbed in the stomach, whereas those soluble in an alkaline environment are absorbed in the small intestine. In bariatric procedures such as RYGB or SG, the acid-producing cells in the fundus are excised or partitioned off, leading to decreased production of hydrochloric acid and an increase in gastric pH. Gastric pH is also increased with the use of proton pump inhibitors (PPI’s), such as lansoprazole or omeprazole, which is common after bariatric procedures.
This may affect the dissolution rate of specific drugs[26],[28]
and, theoretically, could increase solubility of certain medications (e.g. allopurinol, i.e. basic drugs), and decrease solubility and absorption of medications dependent on an acidic environment (e.g. acetylsalicylic acid)[26],[27]
. Where possible, switching to a liquid formulation would eliminate the need for drug dissolution and therefore increase absorption. Effects on nutrient absorption may also be observed[26]
. This can be overcome with a different preparation, such as calcium citrate, which does not depend on an acidic environment unlike other forms and has demonstrated an increased bioavailability compared with calcium carbonate[50]
. Additionally, iron is dependent on hydrochloric acid to reduce it to a ferrous form. In order to overcome this, iron supplements can be combined with ascorbic acid[51]
, which have been demonstrated to improve ferritin levels and anaemia.
It is important to consider that the majority of drug absorption occurs in the small intestine as the stomach exhibits a much lower surface area to volume ratio. This makes the significance of reduced gastric pH and absorption unclear[26],[27]
.
Gastric emptying
Following surgery, gastric emptying, which is reliant partially on the pylorus but also affected by peptide YY (see ‘Table 1: Proposed mechanism of bariatric surgery’), is delayed[52]
. This is especially relevant with SG and gastric banding, where the pylorus is preserved and leads to a prolonged and earlier feeling of satiety. This may have implications when administering medications, although the significance is uncertain[27],[37]
. It is suggested the rate of absorption may be reduced but the degree of absorption should remain unchanged[27]
. Commonly, patients who undergo bariatric surgery can usually only tolerate a liquid diet for the first six weeks post-operatively[53]
. Although no guidelines exist, standard practice is to switch to liquid formulations, where possible, until a solid diet is resumed[53]
.
Mucosal exposure
Bypass procedures markedly reduce the surface area available for drugs to be absorbed along the gastrointestinal tract[27],[37]
as a result of loss of villi and microvilli that would normally increase the absorptive area. Through bypassing the proximal small intestine, the largest surface area per unit length of the tract is removed and this leads to lower nutrient and fat absorption, and therefore greater weight loss. However, the distal small intestine, which has a smaller surface area in comparison, has a slower transit time that may aid in increasing drug absorption[26],[27]
.
Drugs with slow dissolution properties (e.g. extended release) are likely to exhibit reduced bioavailability and absorption as a result of a significant portion of the gastric tract being bypassed. This can be important in critical drugs such as antiepileptics (see ‘Table 2: Medications with specific advice following bariatric surgery’). Current recommendations are that these preparations should be avoided, as they may have exited the gastrointestinal tract before absorption is complete[27],[37],[53]
. Overcoming this issue can be achieved by replacing it with immediate release formulations of the same drug. However, a potential disadvantage of this is increased frequency of administration, which could affect patient compliance and adherence.
Lipophylicity
On account of bypass of the biliary system and the restriction of bile-salt mixing with nutrients and drugs to the common channel, drugs that are highly lipophilic may be affected. These are dependent on the presence of bile salts for absorption and usually undergo entero-hepatic recirculation. Lipophilic medications include tacrolimus and levothyroxine, which will need monitoring in this subset of patients (see ‘Table 2: Medications with specific advice following bariatric surgery’).
Transporter systems
Located in numerous sites, including the intestine, liver and kidneys, transporter systems are important in drug absorption and distribution and have complex interactions with drugs. For example, some medications, such as atorvastatin, are substrates for P-glycoprotein, a transporter that has increasing activity in the distal intestine, and through bypassing the main site for absorption this may lead to increased efflux of the drug through the transporter and reduced drug levels. In addition, antibiotics such as the fluoroquinolones depend on the organic anion transporting polypeptide (OATP) influx transporter, and therefore bioavailability may be reduced in bypass procedures because of reduced exposure[54]
.
There is suggestion that compensatory mechanisms may take place leading to unaltered drug absorption, however current evidence is inconclusive[27],[55]
.
Distribution
Drugs with high lipid solubility or low plasma binding have a higher volume of distribution (Vd) and the physical volume of the individual affects this. The other factors that influence drug distribution (e.g. cardiac output and vascular permeability) are not usually affected. Following bariatric surgery, there is profound weight loss and this appears to include both fat mass and lean mass[56]
. There is no evidence that distribution is affected and current recommendations are that doses are calculated according to total body weight for lipophilic drugs and with ideal body weight for those drugs where distribution is mostly to lean body mass[57]
. Accurate monitoring of weight and drug levels where appropriate is advised (see ‘Table 2: Medications with specific advice following bariatric surgery’). Clearance rates should also be regularly monitored, as many patients in this population have pre-existing renal impairment that may improve with weight loss[58]
.
Metabolism
Most drug metabolism occurs in the presence of liver enzymes (e.g Cytochrome P450 oxidases), while some occurs in the small intestine and to a lesser degree (e.g.CYP3A) in the proximal small intestine. However, in the absence of pre-existing liver disease or interacting medications, there is no clear effect of bariatric surgery on drug metabolism[31],[34]
.
Another consideration is the effect on entero-hepatic recirculation. On account of the diminished surface area, there will be reduced initial absorption and subsequent reabsorption also. The overall effect may be reduced drug levels (e.g. lithium), and close monitoring of narrow therapeutic index drug levels is advised (see ‘Table 2: Medications with specific advice following bariatric surgery’).
Other considerations
On account of the reduced gastric capacity following bariatric surgery, there is an observed risk of gastric ulceration in relation to non-steroidal anti-inflammatory drugs[59]
. Marginal ulcers have been reported in up to 16% of patients[59], therefore, standard practice in bariatric centres is avoidance of these agents[53]
. Alternative analgesics include paracetamol, tramadol or oramorph, which are available as liquid preparations.
Studies show a prevalence of nutrient and vitamin deficiency in 50–69% of post-operative patients[60]
, likely caused by reduced mucosal exposure and bile-salt mixing. Therefore, international (American Association of Clinical Endocrinologists, The Obesity Society and American Society for Metabolic and Bariatric Surgery) and UK (British Obesity and Metabolic Surgery Society) guidelines[61],[62]
suggest close monitoring of folate, B12, ferritin, calcium, vitamin D, zinc and copper as routine. Multivitamins are recommended following all bariatric procedures but RYGB and SG have higher requirements. Specifically, it is recommended patients take 2mg copper, 45–50mg iron (100mg if menstruating), 800–1200mg calcium and 20µg vitamin D daily. Thiamine should be considered with prolonged vomiting post-operatively and a three-monthly vitamin B12 injection is advised[61]
. This is because the bypass of gastric parietal cells causes a lack of intrinsic factor, leading to malabsorption of oral vitamin B12. In addition, bisphosphonates present a risk of gastric ulceration because of the reduced gastric size, and therefore alternatives such as raloxifene or calcitonin nasal spray are advised[37]
.
Contraception is an important consideration in the pre-operative and post-operative population. International guidelines advise against oral hormonal contraception because of concerns about absorption. Alternative options are recommended, specifically barrier methods, intrauterine devices, the implant or the contraceptive ring[63]
.
For those wishing to become pregnant, women who are obese or who have undergone bariatric surgery should have pre-conception planning and follow-up in a specialist clinic because of an increased risk of complications. Management includes high-dose folic acid (5mg), vitamins that do not contain vitamin A in the retinol form because of its teratogenic effect, and nutritional screening every trimester[61],[62]
.
Catherine Huang, MRCP MBCHB, is a specialist trainee, critical care and acute medicine, Royal London Hospital, London, UK. Farokh Master is clinical pharmacist, critical care department, University College Hospital London.
Reading this article counts towards your CPD
You can use the following forms to record your learning and action points from this article from Pharmaceutical Journal Publications.
Your CPD module results are stored against your account here at The Pharmaceutical Journal. You must be registered and logged into the site to do this. To review your module results, go to the ‘My Account’ tab and then ‘My CPD’.
Any training, learning or development activities that you undertake for CPD can also be recorded as evidence as part of your RPS Faculty practice-based portfolio when preparing for Faculty membership. To start your RPS Faculty journey today, access the portfolio and tools at www.rpharms.com/Faculty
If your learning was planned in advance, please click:
If your learning was spontaneous, please click:
References
[1] World Health Organization. Obesity: Preventing and managing the global epidemic 2004. Available at: www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/ (accessed February 2016).
[2] Ng M, Fleming T, Robinson M et al. Global, regional and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet 2014;384:766–781. doi: 10.1016/S0140-6736(14)60460-8
[3] The British Obesity and Metabolic Surgery Society. The National Bariatric Surgery Registry. Second Registry Report 2014. Available at: http://www.bomss.org.uk/wp-content/uploads/2014/04/Extract_from_the_NBSR_2014_Report.pdf (accessed February 2016).
[4] Adams KF, Schatzkin A, Harris TB et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. New England Journal of Medic ine 2006;355:763–778. doi: 10.1056/NEJMoa055643
[5] Calle EE, Rodriguez C, Walker-Thurmond K et al. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. New England Journal of Medicine 2003;348:1625–1638. doi: 10.1056/NEJMoa021423
[6] Health and Social Care Information Centre. Statistics on obesity, physical activity and diet: England 2015. Available at: http://www.hscic.gov.uk/catalogue/PUB16988/obes-phys-acti-diet-eng-2015.pdf (accessed February 2016).
[7] Moody A. Adult anthopometric measures, overweight and obesity — England. The Health and Social Care Information Centre. 2013.
[8] World Health Organization. Global Health Observatory Data Repository. Available at: http://apps.who.int/gho/data/node.main.A900A?lang=en480A?lang=en (accessed February 2016).
[9] Butland B, Jebb S, Kopelman K et al. Foresight. Tackling obesities: future choices. Project report 2007. Available at: www.gov.uk/government/uploads/system/uploads/attachment_data/file/287937/07-1184x-tackling-obesities-future-choices-report.pdf (accessed February 2016).
[10] Public Health England. Economics of obesity. Available at: www.noo.org.uk/NOO_about_obesity/economics (accessed February 2016).
[11] Picot J, Jones J, Colquitt JL et al. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health Technology Assessment 2009;13(41). doi: 10.3310/hta13410
[12] American Society for Metabolic and Bariatric Surgery. Metabolic and Bariatric Surgery Fact Sheet 2013. Available at: https://asmbs.org/resources/metabolic-and-bariatric-surgery (accessed February 2016).
[13] Sjostrom L, Lindroos AK, Peltonen M et al. Lifestyle, diabetes and cardiovascular risk factors 10 years after bariatric surgery. New England Journal of Medicine 2004;351:2683–2693. doi: 10.1056/NEJMoa035622
[14] The Longitudinal assessment of bariatric surgery (LABS) Consortium. Peri-operative safety in the longitudinal assessment of bariatric surgery. New England Journal of Medicine 2009;361:445–454. doi: 10.1056/NEJMoa0901836
[15] Livingston EH. Procedure incidence and in-hospital complication rates of bariatric surgery in the United States. American Journal of Surgery 2004;188:105–110. doi: 10.1016/j.amjsurg.2004.03.001
[16] The National Institute for Health and Care Excellence. Obesity: Identification, assessment and management of overweight and obesity in children, young people and adults 2014. Available at: www.nice.org.uk/guidance/cg189 (accessed February 2016).
[17] NHS England. Clinical commissioning policy: Complex and Specialised obesity Surgery 2013. Available at: www.england.nhs.uk/wp-content/uploads/2013/04/a05-p-a.pdf (accessed February 2016).
[18] Sjostrom L, Peltonen M, Jacobsen P et al. Bariatric surgery and long-term cardiovascular events. Journal of the American Medical Association 2012;307:56–65. doi: 10.1001/jama.2011.1914
[19] Puzziferri N, Roshek TB, Mayo HG et al. Long term follow up after bariatric surgery: A systematic review. Journal of American Medical Association 2014;312:934–942. doi: 10.1001/jama.2014.10706
[20] Ionut V & Bergamn RN. Mechanisms responsible for excess weight loss after bariatric surgery. Journal of Diabetes Science and Technology 2011;5:1263–1282. doi: 10.1177/193229681100500536
[21] Le Roux CQ, Welbourn R, Werling M et al. Gut hormones as mediators of appetite and weight loss after Roux-en-y gastric bypass. Annals of Surgery 2007;246:780–785. doi: 10.1097/SLA.0b013e3180caa3e3
[22] Peterli R, Wolnerhanssen B & Peters T. Improvement in glucose metabolism after bariatric surgery: comparison of laparoscopic Roux-en-y gastric bypass and laproscopic sleeve gastrectomy: a prospective randomised trial. Annals of Surgery 2009;250:234–241. doi: 10.1097/SLA.0b013e3181ae32e3
[23] Le Roux CW, Borg C, Wallis K et al. Gut hypertrophy after gastric bypass is associated with increased glucagon-like peptide 2 and intestinal crypt cell proliferation. Annals of Surgery 2010;252:50–56. doi: 10.1097/SLA.0b013e3181d3d21f
[24] Laferrere B, Swerdlow N, Bawa B et al. Rise of oxyntomodulin in respopnse to oral glucose after gastric bypass surgery in patients with type 2 diabetes.Journal of Clinical Endocrinology and Metabolism 2010;95:4072–4076. doi: 10.1210/jc.2009-2767
[25] Kral JG, Gortz L, Hermansson G et al. Gastroplasty for obesity: long-term weight loss improved by vagotomy.World Journal of Surgery 1993;17:75-79. doi: 10.1007/BF01655710
[26] Sawaya RA, Jaffe J, Friedenberg L, Friedenberg FK. Vitamin, mineral, and drug absorption following bariatric surgery. Current Drug Metabolism 2012;13:1345-55. doi: 10.2174/138920012803341339
[27] Padwal R, Brocks D, Sharma AM. A systematic review of drug absorption following bariatic surgery and its theoretical implications. Obesity Reviews 2010;11:41-50. doi: 10.1111/j.1467-789X.2009.00614.x
[28] Seaman JS, Bowers SP, Dixon MS, Schindler L. Dissolution of common psychiatric medication in a roux-en-y gastric bypass model. Psychosomatics 2005;46:250-253. doi: 10.1176/appi.psy.46.3.250
[29] BPNG data on file. http://www.bpng.co.uk/
[30] Fysekidis M, Cohen, R, Beheit M et al. Sleeve gastrectomy is a safe and efficient procedure in HIV patients with morbid obesity: a case series with results in weight loss, comorbidity evolution, CD4 counts and viral load. Obesity Surgery 2015;25:229–233. doi: 10.1007/s11695-014-1350-7
[31] Edwards A & Ensom MHH. Pharmacokinetic effects of bariatric surgery. Annals of Pharmacotherapy 2012;46:130–136. doi: 10.1345/aph.1Q414
[32] Skottheim IB, Stormark K, Christensen H et al. Significantly altered systemic exposure to atorvastatin acid following gastric bypass surgery in morbidly obese patients. Clinical Pharmacology and Therapeutics 2009;86:311–318. doi: 10.1038/clpt.2009.82
[33] Pfizer. Summary of Product Characteristics.
[34] Hamad GG, Helsel JC, Perel JM et al. The effect of gastric bypass on the pharmacokinetics of serotonin reuptake inhibitors. American Journal of Psychiatry 2012;169:256–263. doi: 10.1176/appi.ajp.2011.11050719
[35] Cipramil Drops (Lundbeck), Summary of Product Characteristics. January 2012.
[36] Lanoxin PG Elixir (Aspen), Summary of Product Characteristics. November 2013.
[37] Miller AD & Smith KM. Medication and nutrient administration considerations after bariatric surgery. American Journal of Health-System Pharmacy 2006;63:1852–1857. doi: 10.2146/ajhp060033
[38] Prozac, Summary of Product Characteristics; March 2013.
[39] Lamictal Combined Tablets (GSK), Summary of Product Characteristics; February 2013.
[40] Levothyroxine (Celltech), Summary of Product Characteristics; October 2001.
[41] Priadel (Sanofi-Aventis), Summary of Product Characteristics; January 2014.
[42] Padwal RS, Gabr RQ, Sharma AM et al. Effect of gastric bypass surgery on the absorption and bioavailability of metformin. Diabetes Care 2011;34:1295–1300. doi: 10.2337/dc10-2140
[43] Rosemont. Summary of Product Characteristics.
[44] Lopresor Tablets (Recordati), Summary of Product Characteristics. October 2010.
[45] Arzip (Winthrop Pharma), Summary of Product Characteristics. November 2010.
[46] Zyprexa (Lilly), Summary of Product Characteristics. 27 May 2013.
[47] Losec MUPS (AstraZeneca), Summary of Product Characteristics. 21 May 2013.
[48] Paroxetine (Sandoz), Summary of Product Characteristics. December 2015.
[49] Astellas. Summary of Product Characteristics.
[50] Tondapu P, Provost D, Adams-Huet Bet al. Comparison of the absorption of calcium carbonate and calcium citrate after Roux-en-y gastric bypass.Obesity Surgery 2009;19:1256–1261. doi: 10.1007/s11695-009-9850-6
[51] Rhode BM, Shustik C, Christou NV et al. Iron absorption and therapy after gastric bypass. Obesity Surgery 1999;9:17–21. doi: 10.1381/096089299765553656
[52] Horowitz M, Cook DJ, Collins PJet al. Measurement of gastric emptying after gastric bypass surgery using radionuclides. British Journal of Surgery 1982;69:655–657. doi: 10.1002/bjs.1800691108
[53] PrescQIPP. Bariatric patients and their medicines. Available at: https://www.prescqipp.info/resources/viewcategory/226-bariatric-patients-and-their-medicines (accessed Nov 2015).
[54] Maeda T, Takahashi K, Ohtsu N et al. Identification of influx transporter for the quinolone antibacterial agent levofloxacin. Molecular Pharmacology 2007;4:85–94. doi: 10.1021/mp060082j
[55] Zhou SF. Structure, function and regulation of P-glycoprotein and its clinical relevance in drug disposition. Xenobiotica 2008;38:802–832. doi: 10.1080/00498250701867889
[56] De Aquino LA, Pereira SE, de Souza Silva J et al. Bariatric surgery: impact on body composition after Roux-en-Y gastric bypass. Obesity Surgery 2012;22:195–200. doi: 10.1007/s11695-011-0500-4
[57] Macgregor AMC & Boggs L. Drug distribution in obesity and following bariatric surgery: a literature review. Obesity Surgery 1996;6:17–27. doi: 10.1381/096089296765557222
[58] Ejerblad E, Fored CM, Lindblad P et al. Obesity and risk for chronic renal failure. Journal of the American Society of Nephrology 2006;17:1695–1702. doi: 10.1681/ASN.2005060638
[59] El-Hayek K, Timratana P, Shimizu Het al. Marginal ulcer after Roux-en-Y gastric bypass: what have we really learned? Surgical Endoscopy 2012;26:2789–2796. doi: 10.1007/s00464-012-2280-x
[60] Slater GH, Ren CJ, Siegel N et al. Serum fat-soluble vitamin deficiency and abnormal calcium metabolism after malabsorptive bariatric surgery. Journal of Gastrointestinal Surgery 2004;8:48–55. doi: 10.1016/j.gassur.2003.09.020
[61] British Obesity and Metabolic Society. Guidelines on peri-operative and post-operative biochemical monitoring and micronutrient replacement for patients undergoing bariatric surgery. Available at: http://www.bomss.org.uk/wp-content/uploads/2014/09/BOMSS-guidelines-Final-version1Oct14.pdf (accessed February 2016)
[62] Mechanick JI, Youdim A, Jones DB et al. Perioperative nutritional, metabolic, and non surgical support of the bariatric surgery patient – 2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity society, and American Society for Metabolic and Bariatric Surgery. Endocrine Practice 2013;19:337–372. doi: 10.4158/EP12437.GL
[63] Center for Disease Control and Prevention. U.S. Medical eligibility criteria for contraceptive use 2010. Available at: http://www.cdc.gov/mmwr/pdf/rr/rr59e0528.pdf (accessed February 2016).


