
Eye of Science / Science Photo Library
Summary box
In this article you will learn:
- The common causes of dentine sensitivity
- The anatomy of a tooth and how it relates to sensitivity
- How sensitivity toothpastes and mouthwashes work
- When to refer a patient to a dentist
Dentine hypersensitivity, or sensitive teeth, is a common condition[1]
. In a recent study of 3,187 adults across Europe, 40% self-reported a painful response to cold air and, on examination, 60% were found to have at least one sensitive tooth[2]
.
It affects people of all ages and most people suffer at some time in their life. It is most common in people aged 18–35 years, and is more common in women[2]
. There is growing evidence that dentine hypersensitivity has become more common in older people, many of whom are retaining more teeth throughout life.
Typically, sensitivity occurs in response to cold stimuli such as ice cream or cold drinks, but can also be caused by hot or sugary foods, or by direct contact or pressure. The characteristic sharp pain is instantaneous and lasts for a few seconds, and once the cold stimulus is removed, the discomfort subsides, typically within a few seconds[3]
. The upper and lower anterior and premolar teeth are most commonly affected. Sensitive tooth pain is often intermittent, which may be related to changes in diet or tooth brushing habits.
Dentine hypersensitivity is diagnosed after other common causes of sensitivity are eliminated (e.g. dental caries, cracked teeth, pain after a filling).
Misdiagnosis and inappropriate treatment may result in unnecessary discomfort, and increase risk of worsening the underlying cause, which can result in the patient requiring dental surgery. Therefore all patients presenting with tooth sensitivity for the first time should be referred to a dentist.
Causes
Intact teeth are covered by an outer shell of enamel, which is up to 2–3mm thick, overlying an inner core of dentine. The dentine surrounds and protects the pulp of the tooth, which includes the nerves and blood supply that maintain the vitality of the tooth.
Dentine is full of millions of minute tubules, running from the pulp to the junction between the dentine and enamel, linking the dental pulp to the inner surface of the enamel. The tubules, which are only a few micrometres wide, contain a delicate extension of a pulpal cell tissue bathed in a fluid, which can move along the lumen of the tubule.
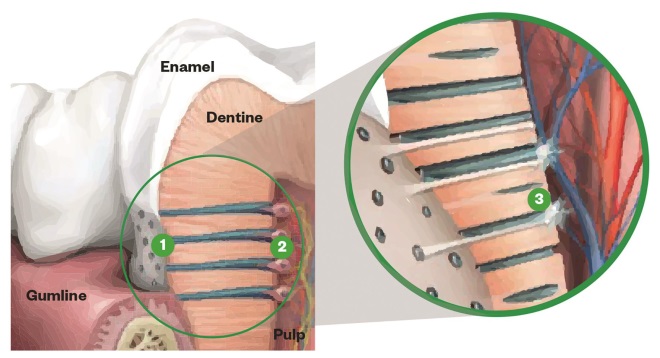
Anatomy of a tooth
Source: Image Courtesy of GSK
Dentine hypersensitivity is caused by the exposure of dentinal tubules to the interior of the mouth. 1) Tubules: dentine contains millions of tubules a few micrometers wide. 2) Tubule lumen: the tubules contain pulpal cell tissue bathed in a fluid. 3) Sensitivity: pain can occur when the tubules are exposed and the fluid in the lumen moves
If tubules are exposed to the inside of the mouth, the fluid in them moves in response to various stimuli and excites the nerves of the dental pulp, provoking a painful response.
If intact teeth are supported by healthy gums, the enamel and gum (gingival) margins block the end of the dentinal tubules and stop anything causing the movement of the dentinal tubule fluid[4]
. Therefore, individuals with intact teeth and healthy gums do not tend to suffer from sensitive teeth. If enamel is lost or removed (i.e. because of dental caries), or gingival tissues recede because of gum disease, the dentinal tubules are exposed and the risk of sensitivity is increased.
Acids present in the diet also have the potential to dissolve the enamel and expose the underlying dentine. A recent study in seven European countries found around 30% of adults had signs of acid erosion[2]
. Once the enamel is lost, it cannot be reformed and the risk of sensitivity increases.
Exposed dentine does not always result in dentine hypersensitivity. There is a natural blocking mechanism called the smear layer. This layer, which comprises proteins in saliva and mineral debris from teeth lost through normal wear and tear, readily develops over the surface of exposed dentine, forming a barrier to the stimuli that can cause dentine hypersensitivity. The smear layer is able to withstand the everyday rigours of the oral environment and, if damaged, is restored relatively quickly.
However, in patients who regularly consume acidic foods or drinks, the smear layer may break down and does not have time to be restored, increasing the risk of dentine hypersensitivity. This is also a risk in patients who have overzealous tooth brushing habits, particularly if they have an inappropriate tooth brushing technique (e.g. vigorous horizontal ‘scrubbing’).
There is not usually an association between the location of the sensitivity and left- or right-handed tooth brushing, or the severity of the sensitivity whether a hard or soft toothbrush is used.

Extreme cases of tooth erosion causing dentine hypersensitivity
Source: Courtesy of Nairn Wilson
1) Erosion of the upper anterior teeth which have become shortened and suffered incisal (biting edge) chipping, causing sensitivity. This cannot be managed by the use of an over-the-counter product. 2) Damage to the necks of upper anterior and premolar teeth with a large amount of exposed dentine.
Desensitising products
Desensitising toothpastes and mouthwashes aim to reduce the pain associated with dentine hypersensitivity. The active agents either interfere with nerve transmission in the dentinal tubules, reducing or eliminating the sensation of sensitivity in the pulp, or form, through precipitation, a coating over the outer surface of the teeth that acts as an artificial smear layer and occludes the open dentinal tubules[5]
.
Nerve transmission blockers contain nitrites, typically potassium nitrite, which gradually permeates down the tubules to interrupt the transmission of nerves contained in the dentinal tubules. These toothpastes, in common with other forms of desensitising toothpaste, tend to work slowly over a few weeks, with the maximum benefit building up over time rather than occurring quickly.
Clinical studies have confirmed the effectiveness of these toothpastes, subject to users adhering strictly to the directions for use over the time required for the active ingredient to take effect[5]
.
Artificial, smear layer toothpastes cover exposed dentine surfaces, including open dentinal tubules, and block the movement of the fluid in the dentinal tubules. These artificial barriers typically comprise calcium-containing ingredients and all have a similar mechanism. The barrier usually takes up to two weeks to build up and needs to be replenished on a daily basis to maintain its effectiveness.
There is no strong evidence to suggest either type of product is more effective.
Patient advice
Patients using over-the-counter toothpastes for sensitive teeth should be given advice on good tooth brushing technique and advised to reduce their consumption of acidic food and drink.
Many patients self-medicate to manage the pain associated with dentine hypersensitivity and only seek advice when they experience more severe bouts of pain, or have used over-the-counter products to little effect. This is especially common among people who do not seek regular dental care or who are afraid of going to the dentist.
Pharmacists should refer patients with troublesome, persistent tooth sensitivity to a dentist. The dentist will be able to exclude other, possibly more serious, dental problems and prescribe a series of measures to control and hopefully manage the condition. This may involve periodontal (gum) treatment and sealing or covering over the sensitive surfaces with fillings or crowns. In extreme cases, endodontic treatment — when the nerve of the tooth is removed and the tooth root filled — may be required.
David Bartlett PhD FDS is professor of prosthodontics and
Nairn Wilson PhD FDS is professor of dentistry, both at
King’s College London Dental Institute
References
[1] West NX, Sanz M, Lussi A et al. Prevalence of dentine hypersensitivity and study of associated factors: a European population-based cross-sectional study. J Dent 2013 41:841–851.
[2] Bartlett DW, Lussi A, West NX et al. Prevalence of tooth wear on buccal and lingual surfaces and possible risk factors in young European adults. J Dent 2013;41:1007–1013.
[3] Addy M & West N. Etiology, mechanisms, and management of dentine hypersensitivity. Curr Opin Periodontol 1994;71–77.
[4] Lilja J, Nordenvall KJ & Branstrom M. Dentin sensitivity, odontoblasts and nerves under desiccated or infected experimental cavities. A clinical, light microscopic and ultrastructural investigation. Swed Dent J 1982;6:93–103.
[5] Gillam D, Chesters R, Attrill D et al. Dentine hypersensitivity–guidelines for the management of a common oral health problem. Dent Update 2013;40:514–516, 18–20, 23–24.


