
Kristoffer Stewart / Green Light Pharmacy
The guidance and advice on COVID-19 contained within this article was correct at the time of publication. Guidance has now been updated and there are currently no restrictions in place in the UK. For more information, see: https://www.gov.uk/coronavirus
The Royal Pharmaceutical Society has made this feature article free to access in order to help healthcare professionals stay informed about an issue of national importance. To learn more about coronavirus, please visit: https://www.rpharms.com/resources/pharmacy-guides/wuhan-novel-coronavirus.
Unlike many other public services and businesses, community pharmacies will continue to stay open during the COVID-19 pandemic to deliver essential counselling, information and medicines supply to patients and local communities[1],[2]
.
With a significant increase in demand for medicines, coupled with a change in public behaviour — such as panic buying over-the-counter painkillers in response to the lockdown — this is putting tremendous pressure on pharmacy teams[3],[4]
.
However, community pharmacies are rapidly adapting their frontline service to meet unprecedented demand as the pandemic develops. This article summarises how pharmacists can implement guidance and best practice in response to the rapidly changing pandemic to ensure patient and staff safety, as well as the approaches pharmacy teams across the UK are taking in response to COVID-19.
Aspects covered include:
- Enforcing social distancing;
- Maintaining safe staffing;
- Communicating with patients;
- Keeping your team safe;
- Adjusting opening hours and pharmacy services;
- Ensuring adequate stock;
- Hygiene and infection control measures;
- Maintaining medicines deliveries.
We will be updating this article on a weekly basis with the most recent advice and resources for pharmacy teams. If your community pharmacy has developed a new way of working that is proving successful, please email us with the details, so that we may include it in the article.
1. Enforcing social distancing
Current government guidance advises that all individuals keep two metres apart to prevent passing on COVID-19 infection. Pharmacy teams must consider how they are going to implement controls to enforce this for patients and each other[5]
. The guidance also highlights that particularly stringent social distancing behaviours need to be adopted by those that are high-risk (i.e. those aged 70 years or over, regardless of medical conditions, or those aged under 70 years with an underlying health condition, such as heart disease or diabetes)[5]
.
There is no strict guidance on how social distancing should be implemented in pharmacies, but different pharmacies have attempted to achieve this by:
- Placing physical barriers in doorways or in front of the pharmacy counter to prevent patients from getting close, for example using chairs or tables;
- Cordoning off areas using store shelving to redirect patients;
- Adding tape on the ground to section areas of the pharmacy that patients can stand in to help ensure distance;
- Placing acrylic glass barriers in front of the counter or building hatches for the collection of medicine, which may require the specialist expertise of a joiner.
I finally completed putting up hygiene screens in all 4 pharmacies at huge expense! Everyone feels safer & my teams deserve every bit of protection so they can continue staying open for our patients. â¦@NPA1921â© â¦@PSNCNewsâ© â¦â¦@ChemistDruggistâ© #pharmacyheroes
pic.twitter.com/sv7SKNUBkP— Olivier Picard (@OlivierPicardUK) March 31, 2020

Source: Marc Borson
Perspex barrier added to a pharmacy to help reduce patient contact
Keith Ridge, chief pharmaceutical officer for England, and Ed Waller, director of primary care strategy and NHS Contracts, and lead at NHS England and NHS Improvement, have written to pharmacists, indicating that they will give all pharmacies (who are not distance-selling pharmacies) a £300 payment to support the installation of physical barriers, such as screens and retractable tape barriers or other adjustments to help enforce social distancing.
Examples from community pharmacies in the UK are included in Box 1 and images below.
Box 1: Examples of measures implemented in community pharmacy across the UK to ensure social distancing

Source: Reena Barai
Floor markings can help indicate to patients were they should stand while in the pharmacy

Source: Ade Williams
Floor markings can help indicate to patients the procedure while entering and waiting in the pharmacy

Source: Kristoffer Stewart / Green Light Pharmacy
Providing floor markings can help patients understand where they should stand in the pharmacy to ensure appropriate social distancing
These measures may seem extreme, but have been adopted to help prevent the spread of COVID-19 to employees and between patients, especially those who may be vulnerable to infection or in high-risk groups. In addition, some pharmacies are limiting the number of people who can be present in the pharmacy at any one time (e.g. one in, one out).
This may be practical if several patients turn up to collect their prescriptions at the same time, but it is necessary and serves as a reminder that this is no longer business as usual.
Reducing interactions
Regardless of the precautions taken to protect pharmacy staff, there will likely be some interaction with patients, such as when handing them their medicines or when taking payments for prescriptions. Other measures, such as encouraging patients to pay using contactless payment, where possible, or placing money in baskets/bowls, may further reduce the need for physical contact.
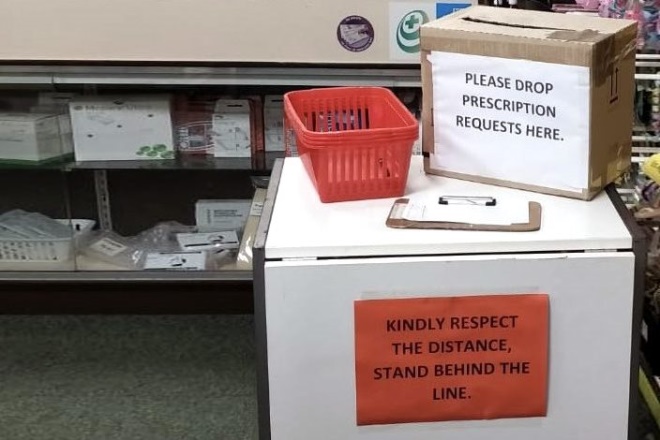
Source: Ade Williams
An alternative way of putting forward prescription requests helps prevent contact between patients and pharmacy staff
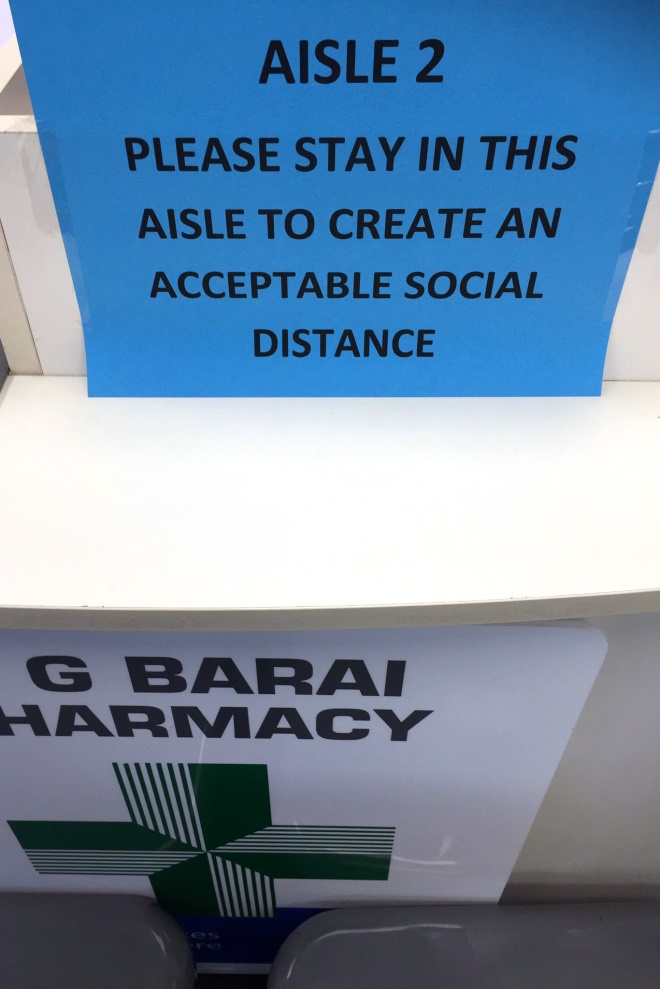
Source: Reena Barai
Creating specific aisles in the pharmacy for patients to stand in can help encourage appropriate social distancing
In addition, the pharmacy may want to operate a shopping service, where patients call to ask for items and then collect them, limiting patient interaction and time spent on the premises; however, the ability to provide this may be limited by the number of staff a pharmacy has available.
Pharmacy teams who are accustomed to working in close confines, for example in a small pharmacy, may need to reconsider how they work. If the store has a small dispensary, but a larger shop area, it may be appropriate to expand the dispensary into the store. This would allow more space between employees. Although this may not be an ideal working environment, it is important to consider if appropriate social distancing is to be maintained. This temporary measure also prevents the number of customers who could enter the store.
2. Maintaining safe staffing
It is important to have a contingency plan if the regular pharmacist is unable to work. This may include:
- Updating your locum list or speaking to locum agencies/booking platforms;
- In England, contacting NHS England and NHS Improvement if the pharmacy is unable to open because a Responsible Pharmacist is unavailable. In Wales, pharmacies should contact their local health authority. In Scotland, the requirement is to contact the local pharmacy services officer in the relative health board;
- Speaking to a neighbouring pharmacy about referring patients to their pharmacy if the one you work in is unable to open;
- In England, speaking to the local primary care network community pharmacy lead who may be able to co-ordinate store closures.
The General Pharmaceutical Council (GPhC) has set out provisions for the supply of pre-dispensed medicines under certain circumstances: “Where no locum cover can be secured at the pharmacy, and recognising the potential effects of the current pandemic, it would be in the patient’s best interest for medicines already dispensed to be supplied from the pharmacy rather than not supplied at all”[6]
.
Essentially, this means that if a pharmacist falls ill and has to leave the pharmacy, medicines that have been dispensed and checked by the pharmacist can be provided to the patient; however, the regulator says that the pharmacy team is expected to have access to a remote pharmacist who could be contacted by phone or video.
If your regular staff are unable to work, it may be appropriate to train staff who work in a different section of the pharmacy to assist in the dispensing of medicines. Alternatively, it may be appropriate to contact former employees to see if they would be willing to work in the pharmacy; however, this should be carefully considered as some employees who have left work may be at a higher risk of COVID-19 if they left because they are retired or owing to ill-health.
Non-regular staff
It is important to consider the needs of staff who are not regularly in the pharmacy. This may inform your decision on how to use them or how you will advise them on current practice. Although standard operating procedures are best practice, the time and resource it would take to create and disseminate this information may not be appropriate. Consider asking non-regular staff to come in early for a briefing of current practice.
It may be appropriate to enlist the help of pharmacy students who have undertaken work experience at the pharmacy in the past. Currently, universities and other higher education institutions have been temporarily closed, so pharmacy students may be able to work part-time while continuing their studies from home. Pharmacy students are also less likely to be in the high-risk group, meaning that they could be suitable temporary staff.
Final year pharmacy students can join their arranged preregistration workplace ahead of the scheduled start date to help deal with the COVID-19 pandemic, according to guidance from six professional bodies. The guidance —published jointly on 9 April 2020 by Health Education England, NHS Education for Scotland, Health Education and Improvement Wales, Pharmacy Schools Council, Royal Pharmaceutical Society (RPS) and the British Pharmaceutical Students’ Association — says that this can be arranged by “mutual consent”. It also emphasises that any deployment of pharmacy students to help with the pandemic must be voluntary and that students should not feel coerced[7]
. See ‘Volunteers’ for more information.
3. Communicating with patients
As pharmacies are likely to be one of the only places on the high street that are still open, patients will continue to require and seek their services, but consideration should be given to how the pharmacy is presented to the public during this period. For example, the retail function of the pharmacy may have to take a step back, with the focus switched to the dispensing of medicines and information.
Store warnings
As a first step, the primary functions of the pharmacy should be shared with the public, for example dispensing medicines and medicine delivery. Placing posters, banners or signs on display in a prominent position is essential in alerting patients about the services the pharmacy can provide at this time. Some pharmacies have found that placing a sign on the door for patients and customers to read before they enter is a suitable way to ensure only those who need to enter the store do so, or may simply set out the limits to the number of people entering at one time (see Box 2 and images below).
Additional information the pharmacy could share may include:
- Latest COVID-19 advice from the government;
- The directions for using the pharmacy or redirecting patients to call the pharmacy with queries rather than turning up in person (i.e. to move away from face-to-face patient consultations);
- The policy for abusive customers (see below).
Box 2: Examples of information for patients

Source: Kristoffer Stewart / Green Light Pharmacy
A sign on a pharmacy counter limiting the number of people who can approach the counter
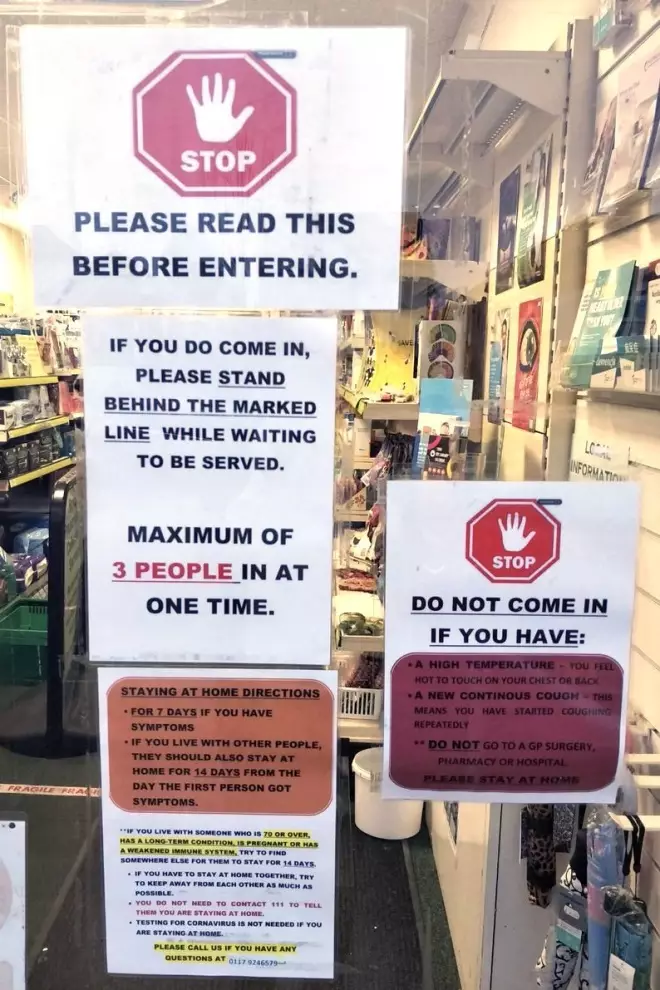
Source: Ade Williams
Placing notifications in shop windows is one method of informing customers of current measures in the pharmacy
It would be beneficial to review any information on display daily to ensure it is up to date and changed to reflect business requirements or government guidance[8]
. In addition, some pharmacies have many posters and notifications on notice boards and in shop windows relating to other topics. It may be necessary to temporarily remove these to prioritise communicating new notifications related to COVID-19 and its management alongside the function of the pharmacy.
If your pharmacy has a social media page or a website, this is another place where guidance should be highlighted. In addition, these pages are a useful tool for sharing information relating to:
- When it is suitable for individuals to visit the pharmacy;
- Advice for patients on how to best manage their health during isolation;
- Access to sick notes for those who are unable to work — you can explain how they can obtain online isolation notes to provide proof of COVID-19-related absence from work;
- Who to contact if patients are concerned about their symptoms (e.g. using NHS 111 online);
- Details on the patient groups that need to self-isolate for 12 weeks (e.g. those with underlying health conditions, pregnant women)[9],[10]
.
Abuse from patients and the public
Sadly, some pharmacies have reported abuse from patients. Whether this is a result of panic or anxiety, it is not acceptable. As such, pharmacies should place signs in their window indicating that patients will not be served if they behave inappropriately.
The RPS has created a poster that can be placed in store windows, indicating that patients may face a longer wait time and that they can help by being patient and polite[11]
. Pharmacy teams who receive abuse should adopt a zero tolerance policy, meaning that you can refuse to serve a particular patient and contact the police if necessary. Some stores have security who are able to remove patients, but for those who do not have this support, they should not endanger themselves. Explain to the patient that they must leave or else you will call the police. If they do not leave, you should follow through on this action. The following should be considered as abuse:
- Using inappropriate language or swearing at staff;
- Any physical violence towards any member of the team or other patients, such as pushing or shoving;
- Verbal abuse towards the staff in any form;
- Racial abuse;
- Sexual harassment;
- Persistent or unrealistic demands that cause stress to staff.
Other considerations
Consider how you will communicate with your patients and what implications this will have on the daily working of the pharmacy business. If you are encouraging patients to call the pharmacy rather than attend, consider:
- Reaching out to local GP surgeries for them to pass this message on;
- Placing notifications in shop windows;
- Sharing details via a text messaging service, if available;
- Posting on a company website or via social media regularly;
- Placing a leaflet alongside the patient’s medicine that is being delivered.
If you know of older and/or vulnerable housebound patients who may not be able to leave the house, it may be appropriate to reach out to them. Although this takes time, it can help identify those in need and you can then refer them to the appropriate person (e.g. their social worker/key worker/a relative etc.).
There may be circumstances where GP surgeries need to close following widespread infection or other COVID-19 concerns[12]
. Speak to local GPs and get an understanding of their continuity plan. This information will be vital because patients will likely contact you when they are unable speak to their GP surgery. There may be examples of surgeries shutting, but individual prescribers may still be able to electronically prescribe remotely. In return, sharing the contigency plans of your pharmacy with the local surgeries and other pharmacies may help ensure patients are able to receive their medicine in a timely manner.
Volunteers
On 24 March 2020, Matt Hancock, health and social care secretary, announced a call for members of the public to volunteer as ‘NHS volunteer responders’, who are able to carry out simple, non-medical tasks to support people in England who have been asked to shield themselves from COVID-19, owing to underlying health conditions[13]
.
Those who sign up to help the NHS through the GoodSam app can be called upon to deliver medicines to patients’ homes on behalf of community pharmacy. The postcode-based app will put out a request to the nearest volunteer who said they are able to provide the service required. When volunteers sign up, they are expected to read advice about delivering medicines[14]
.
Pharmacists can request help for at-risk patients via a call centre run by the Royal Voluntary Service, who will match people who need help with volunteers who live near to them. Some charities will also be able to refer people to this service.
An example of how volunteers from a mother’s fitness group helped Bedminster Pharmacy in Bristol with the delivery of medicines to patients was reported in The Times
[15]
.
Although volunteers may be able to provide much-needed help to pharmacies, there is limited advice on how these individuals will be trained and equipped to ensure safe delivery and care for patients.
4. Keeping your team safe
Pharmacy staff will be required to go above and beyond their role in the coming weeks and months. It is important to consider how you can ensure they continue to be fit to work and are able to fulfil the requirements of their role.
Some staff members will be concerned that their patient-facing role puts them at a higher risk of contracting COVID-19. It is important to be honest about the situation, but advise pharmacy staff on behaviours the team can adopt to minimise risk. In addition, it is important to ensure everyone can work without being overwhelmed and exhausted.
It may be appropriate to introduce a new rota for pharmacy staff, which will:
- Give them opportunities to rotate away from patient-facing tasks;
- Help them develop skills in other sections of the pharmacy, which may be beneficial in the long run if other staff are unable to attend work;
- Ensure workers who are at higher risk — such as those with comorbidities (e.g. chronic neurological or respiratory conditions or diabetes) — have little-to-no direct patient contact (see Vulnerable staff for more information).
These changes may be carried out on an ad hoc basis, but writing them out and sharing them with the team will provide reassurance and an understanding of the duties that need to be carried out.
Ensure staff know that if someone in their household has symptoms of COVID-19, they need to self isolate for 14 days. Many staff may try to continue to work, but you should ensure that they know not to return to work.
Staff testing
Although there have been reports indicating that home testing kits for COVID-19 will soon be available to order from community pharmacies and Amazon. It is not yet clear when the kits will be available or whether pharmacy teams will have access to them.
Jeane Freeman, cabinet secretary for health and sport for the Scottish government, has assured the profession that Scottish community pharmacists will be among the frontline NHS staff to be tested for COVID-19[16]
. In Wales, chief medical officer Frank Atherton has said that frontline NHS healthcare workers in patient-facing roles who are employed in acute medical assessment units; hospital emergency departments; critical or intensive care units; primary care and frontline ambulance staff, would be tested for the virus[16]
. Pharmacists in Wales with symptoms of COVID-19 are able to access testing through their local health board.
In England, the Pharmaceutical Services Negotiating Committee (PSNC) has been pressing the UK government for COVID-19 testing for pharmacists. The RPS has backed the call, with Sandra Gidley, president of the RPS, telling The Pharmaceutical Journal on 19 March 2020: “It’s exercising a lot of people’s minds as community pharmacists are, effectively, the NHS frontline as it’s been pushed back because GPs are closing their doors”[16]
.
Community pharmacists will be able to access testing for COVID-19 as part of a government drive to get frontline NHS staff, who are currently self-isolating, back to work. Although this was implemented from 30 March 2020 for NHS staff in critical care, emergency departments and ambulance services who have been forced to self-isolate at home for 14 days, the PSNC has confirmed that community pharmacists would be included in the new testing programme at eventually.
Some drive-in COVID-19 testing services are available for key worker who meet an eligibility criteria. This testing is currently available at Edgbaston Cricket Ground in Birmingham, West Midlands and Worcester Warriors Rugby Ground in Worcestershire, and includes pharmacy employees and adult members of their households.
Personal protective equipment
Many working in pharmacies have been doing so with personal protective equipment (PPE) while others are not using any[17]
. NHS England has provided a range of PPE to pharmacies and, jointly, with NHS Improvement has advised community pharmacy that gloves, aprons and fluid repellent face masks should be ordered via wholesalers in small quantities, with the intention of being used by staff (i.e. not to be sold to the public)[17]
.
Public Health England (PHE) is regularly updating its guidance on the use of PPE for different healthcare professionals. The most recent update (10 April 2020) recommends that pharmacy staff should only wear PPE, specifically the sessional use of fluid-resistance (Type II) surgical masks, when in “contact with possible or confirmed cases of COVID-19”.
Contrary to PHE advice, the RPS has stated that although social distancing is vital in preventing the spread of COVID-19, it appreciates that this is not practical in all pharmacies, in which case it is sensible to use PPE.
The RPS in Scotland has written to the cabinet secretary for health and sport, indicating the need for adequate supplies of quality PPE for pharmacy teams[18]
.
Vaughan Gething, the Welsh health minister, has said that PPE from the pandemic stockpile had been released to frontline NHS staff, including pharmacies[19]
.
Owing to concerns raised by pharmacy teams, the PSNC has called on PHE to urgently “re-examine” its advice on personal protective equipment (PPE) — that indicates pharmacists should only use PPE for close patient contact — because further supplies of gloves, masks and aprons “will be needed” during the COVID-19 pandemic.
Vulnerable staff
Some staff may be at higher risk if they contract COVID-19, but do not meet the requirements for shielding. Pharmacy teams should consider how they can best utilise these staff members while ensuring their safety.
If the consultation room is clear and not used for patient-facing services, vulnerable staff, or those who live with someone who is vulnerable, may be able to use it to complete vital work that does not require patient or colleague contact (e.g. making up monitored dosage system trays, maintaining phone lines and answering queries).
Prescription collections
Although electronic prescription services (EPS) are widely available across England, there are still a proportion of prescriptions that are still printed and collected from the surgery. It is important that pharmacies consider how these prescriptions can be collected and minimise contact with anyone while doing so[20]
.
Pharmacists should speak with the local GP surgery and ask them to provide NHS repeat dispensing services or post-dated prescriptions, including EPS[21],[22]
. In addition, sending prescription requests to the surgery using an ‘NHS.net’ email will create an audit trail.
In Scotland, the electronic transfer of prescriptions, where prescription information is sent electronically from the GP practice to community pharmacies alongside barcoded print prescriptions that are given to the patient, is in place. In response to COVID-19, pharmacists should be aware that GPs may now send paper prescriptions directly to the designated pharmacy.
5. Adjusting opening hours and pharmacy services
There have been reports of pharmacies opening early, working over lunch and closing late in order to meet the current demands during this crisis.
Pharmacists in Scotland have been urged to do what they can to ensure that pharmacies stay open for seven days per week during the COVID-19 crisis[23]
. Whereas in Wales, Gething has sent a message to pharmacies (see Box 3), saying that they are now allowed to open an hour later and earlier, and close for up to two hours during the day.
Box 3: Vaughan Gething’s message to pharmacies on opening hours
A joint statement from the PSNC, Company Chemists’ Association, National Pharmacy Association and Association of Independent Multiple Pharmacies has offered pharmacies flexibility with their opening hours[24]
. This means pharmacies can close for 2.5 hours a day, as long as they are open between 10:00–12:00 and 14:00–16:00pm, as a minimum for stores contracted to core or supplementary hours. For those with 100-hour contracts, they should be open from 10:00–12:00 and 14:00–18:00 as a minimum. However, the pharmacy must have a sign on the door indicating how people can contact the store if urgent help is needed.
Although this flexibility will allow time for staff to take a break, many may try to use it to catch up on other ‘jobs’ that need completing. Pharmacy teams should make sure they take this time to have a break. This is essential to ensure that staff are able to continue working and serving the customers. If breaks are not taken, there is significant risk of physical and mental exhaustion that will result in downstream impact for patient care.
The joint statement highlights that the changes to operating hours “should help to ensure that pharmacies can stay open to the public, and that staff can work safely and are not fatigued by the current high workload and pressures associated with the COVID-19 outbreak. Pharmacy contractors are encouraged to make use of the provisions to support their staff”[24]
.
Store closures
The need for stores to close has been acknowledged by NHS England and NHS Improvement, for example, when staff are unavailable to work[24]
. They indicate that they need to be contacted and informed immediately, and that the pharmacy’s NHS 111 directory services profile is updated. NHS England and NHS Improvement also encourage the use of “buddy arrangements” to help encourage local pharmacies to maintain continuity of service[24]
. The full standard operating procedure can be found here
[25]
.
Pharmacy services
The PSNC has made an agreement to postpone some contracted services within community pharmacy[26]
. This announcement detailed the postponement of services such as hepatitis C testing, blood pressure testing, smoking cessation support and point-of-care testing. The national roll-out of GP referrals to community pharmacy through the community pharmacist consultation service has also been delayed, although the existing pilot will remain in place[26]
.
The implementation of structured medication reviews and the medicines optimisation service specification through primary care networks has also been postponed.
In Wales, the community pharmacy sore throat test-and-treat service has been suspended, as has the ‘medicines use review’ service.
The PSNC is also introducing an ‘NHS urgent medicines supply service’, which will allow patients, whose GP surgery has closed, to continue receiving their medicines without a prescription. The service will be “switched on” locally as needed – this has already happened in some locations.
You may need to reconsider how you carry out consultations, as face-to-face contact should be avoided. However, there is still a need to provide vital information in addition to its supply role.
Telephone consultations may be appropriate, but this may depend on factors such as having multiple phone lines to the pharmacy. Some pharmacies may be able to use mobile phones of staff to make outgoing calls, if the landline is likely to be busy (e.g. owing to large numbers of queries).
With any changes, there are likely to be teething issues, so creating a shared document (e.g. Google Docs) that highlights the issues faced and includes suggestions on how to overcome them — and that can be accessed and edited by anyone in the team — may help others in the team manage better in the future. In addition, organising daily team meetings and debriefing sessions, of no longer than five minutes, may be beneficial.
Pharmacies that deliver a supervised consumption service can withdraw supervised consumption of opioid substitution therapy to reduce the risk of COVID-19 spread[24]
. However, this will be taken on a case-by-case basis by the pharmacist and certain vulnerable patients will continue to be provided medicine. The PSNC has indicated that particular thought should be given to patients receiving services, such as supervised consumption or monitored dosage systems. Consideration can be given to providing daily doses, rather than supervised consumption, on an individual patient risk-assessed basis[24]
.
6. Ensuring adequate stock
Although there will be desires for the pharmacy to continue functioning as a business, it may be appropriate to prioritise what the store is selling. Each individual team will need to prioritise what their local community requires, but the GPhC is helping when certain, essential items are unavailable, for example, if standard packs of paracetamol have sold out, large packs of paracetamol may be split to be sold as standard pack sizes[27],[28]
.
Consider limiting the quantity of items that can be sold from the pharmacy. This should be taken on a case-by-case basis, for example, one individual could be coming to collect medicine for older relatives who are unable to leave the house and so it may be acceptable to provide multiple items to one individual for this reason.
For prescription items, consider what you will do if you are in short supply of an item, whether you have the means to quickly contact the prescriber to make amendments, or with another local pharmacy that may be able to provide the patient with the item. Alternatively working with the GP to inform them when there are shortages so that they can plan what alternatives they can prescribe. In addition, if you have changed your practice for providing prescription owings explain this clearly to patients; for example, the pharmacy may call them when a prescription is ready to be collected, rather than them coming to the premises to check if it is ready. This could help prevent unnecessary contact in the pharmacy.
Tote boxes
Wholesalers have indicated that they have a shortage of tote boxes and, as such, have asked pharmacies to return them as soon as possible to allow them to continue their supply function[29]
. This may be difficult as some teams may not have the time to put away a delivery before a new one arrives; however, efforts should be put in place to ensure that stock is in its correct location, this not only helps return totes, but establishes a safer working environment.
7. Hygiene and infection control measures
Remind staff of the rules relating to basic handwashing. This may seem like an assumed skill, but it is important to ensure everyone is following the guidance produced by the RPS[30]
. To reinforce this message, it may be appropriate to have them observe your handwashing technique; although this may appear condescending, it helps emphasise how hands should be washed to prevent the spread of infection.
Consider implementing policies in the pharmacy relating to uniforms, such as whether staff need to wash their uniforms daily. You could also consider whether you can provide more uniforms for staff.
Although the provision of PPE is sporadic, consideration should be given to what the team are wearing. For example all staff should:
- Wear short sleeves (or rolled-up sleeves);
- Refrain from wearing ties;
- Remove wristwatches or jewellery when in the pharmacy — this not only helps prevent the transmission of COVID-19, but will also help with handwashing that encourages inclusion of the wrist.
Cleaning the pharmacy
Although it is important to clean the pharmacy on a regular basis, this should now be completed more regularly, with extra attention being given to areas that increase the risk of spread (e.g. counter tops, door handles and pens). In addition, reaching out to companies that will conduct a deep clean may be appropriate and you should discuss requirements for a pharmacy premises. PHE has guidance for environmental cleaning following a possible case that covers preparation, the cleaning process and cleaning reusable equipment[31]
.
While completing the general cleaning of the pharmacy you should:
- Use disposable cloths, paper roll or mop heads when possible;
- Clean and disinfect all hard surfaces, floors, chairs and door handles;
- Use detergent disinfectant;
- Regularly wipe down ‘high-touch’ areas (e.g. light switches, refrigerator doors, drawer pulls, sink handles, soap dispensers).
Wearing gloves would be appropriate as the substance you use to clean may be harmful. These gloves should then be washed if you are going to re-use them.
Waste management
Ensure that stores have enough waste bins. Precautions such as double-bagging used tissues or disposable cleaning cloths and separating them from other waste for 72 hours before placing in external waste bins may be necessary[32]
.
8. Maintaining medicines deliveries
Depending on the measures your pharmacy has taken, you may have a higher number of medicines that require delivery to patients. It is important to carry out a risk assessment and ensure that delivery drivers have access to the following, if they require it:
- Information on whether patients are in a high-risk group;
- Enough contracted hours to manage the new workload;
- Protective equipment, such as gloves and wipes;
- Capacity to deliver non-medical products for vulnerable patients, such as toilet roll and soap;
- Training (e.g. shadowing) for new delivery drivers in case the original driver is unable to work;
- The ability to call patients to ensure they are in for delivery, or make decisions to ensure medicine can be safely delivered, such as obtaining permission to deliver it through a post box.
Some delivery companies have initiated new ways of working. For example, Deliveroo — a food delivery service — now offers a no-contact drop off service where they alert the individual that their order has arrived and leave it outside the property to ensure no physical contact takes place[33]
. Actions like this may be necessary when delivering prescriptions to patients who are self-isolating owing to suspected COVID-19 infection or who are vulnerable to infection; however, this would need to be adjusted to ensure the safe delivery of a medicine.
As it will be a busier period in the pharmacy, it is important to track the location of items in the pharmacy. The RPS recommends that “a robust audit trail should be available to confirm successful delivery of the medicine to the person”, but adds that pharmacy teams should consider how they will do this as direct contact for signatures should be avoided[11]
.
Importantly, the government has announced plans to help fund a delivery service for pharmacies, so that the most vulnerable patients are able to receive timely access to their medicines[34]
. Details for how these services are being delivered in England, Scotland and Wales are available here.
Signing the prescription
Many pharmacies have made the choice to sign the patient’s prescription for them to prevent the spread of infection. There is a question of legality when it comes to this practice and the consequences if this takes place. This issue is governed by the ‘Law of agency’ that states that a representative, in this case the pharmacy, acts as if they are an extension of the patient[35]
.
Consequently, any liabilities or penalties incurred by acting as an ‘agent’ are liabilities of the patient. The patient is the original source and, if the information is incorrect, the patient is liable, not the pharmacy. The pharmacy team member would need to ensure that the patient is aware that they are signing the prescription on their behalf and must indicate their exemption. In the past, when a patient’s prescription was signed by the pharmacist, even though they were not entitled to exemption of charges, the NHS has sought repayments[36]
.
- This article was updated on 22 April 2020 to reflect current guidance on COVID-19 for pharmacy teams.
References
[1] Gov.uk. PM statement on coronavirus: 16 March 2020. Available at: https://www.gov.uk/government/speeches/pm-statement-on-coronavirus-16-march-2020 (accessed April 2020)
[2] Gov.uk. PM statement on coronavirus: 18 March 2020. Available at: https://www.gov.uk/government/speeches/pm-statement-on-coronavirus-18-march-2020 (accessed April 2020)
[3] Andalo, D. ‘Unprecedented demand’ for OTC painkillers as COVID-19 outbreak spreads. Pharm J online. 2020. doi: 0.1211/PJ.2020.20207830
[4] BBC. Coronavirus: Europe looking to extend virus lockdowns. 2020. Available at: https://www.bbc.co.uk/news/world-europe-51959243 (accessed April 2020)
[5] UK Government. Guidance on social distancing for everyone in the UK. 2020. Available at: https://www.gov.uk/government/publications/covid-19-guidance-on-social-distancing-and-for-vulnerable-people/guidance-on-social-distancing-for-everyone-in-the-uk-and-protecting-older-people-and-vulnerable-adults (accessed April 2020)
[6] General Pharmaceutical Council and Pharmaceutical Society of Northern Ireland. Regulatory approach in challenging circumstances - GPhC and PSNI joint statement. Available at: https://www.pharmacyregulation.org/news/regulatory-approach-challenging-circumstances-gphc-and-psni-joint-statement?utm_campaign=covid19-gphc-psni-joint-statement-mar-20&utm_source=mailchimp&utm_medium=email (accessed April 2020)
[7] Health Education England. Joint Guidance: Facilitating deployment of pharmacy undergraduate students to support the pharmacy workforce2020. Available at: https://www.hee.nhs.uk/sites/default/files/documents/MPharm%20student%20deployment%20joint%20guidance%20FINAL.pdf (accessed April 2020)
[8] UK Government. Coronavirus (COVID-19): what you need to do. 2020. Available at: https://www.gov.uk/coronavirus (accessed April 2020).
[9] UK Government. Online isolation notes launched — providing proof of coronavirus absence from work. 2020. Available at: https://www.gov.uk/government/news/online-isolation-notes-launched-providing-proof-of-coronavirus-absence-from-work (accessed April 2020)
[10] UK Government. Press release: Major new measures to protect people at highest risk from coronavirus. 2020. Available at: https://www.gov.uk/government/news/major-new-measures-to-protect-people-at-highest-risk-from-coronavirus (accessed April 2020)
[11] Royal Pharmaceutical Society. Coronavirus (COVID-19) Pharmacist updates and information. 2020. Available at: https://www.rpharms.com/coronavirus/ (accessed April 2020)
[12] Wilkinson E. Pharmacy reopens after deep clean amid coronavirus concerns at medical centre. Pharm J online. 2020. doi: 10.1211/PJ.2020.20207698
[13] NHS England. Your NHS needs YOU – Join the NHS Volunteer Responders. 2020. Available at: https://www.england.nhs.uk/participation/get-involved/volunteering/nhs-volunteer-responders/ (accessed April 2020)
[14] Wickware C. Community pharmacies to use volunteers for patient medication deliveries. Pharm J online. 2020. doi: 10.1211/PJ.2020.20207854
[15] Malvern J. Drug runners keep medicines moving during lockdown. 2020. Available at: https://www.thetimes.co.uk/article/drug-runners-keep-medicines-moving-during-lockdown-5khm9lxxj (accessed April 2020)
[16] COVID-19 latest: Health minister urges patients not to request home medicines deliveries. Pharm J March 2020 online. Available at: https://www.pharmaceutical-journal.com/news-and-analysis/news-blog/covid-19-latest-health-minister-urges-patients-not-to-request-home-medicines-deliveries/20207843.article (accessed April 2020)
[17] NHS England and NHS Improvement. Letter to community pharmacy. 2020. Available at: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/preparedness-letter-primary-care-pharmacy-9-march.pdf (accessed April 2020)
[18] Royal Pharmaceutical Society Scotland. RPS in Scotland asks for further support and recognition for pharmacy teams. 2020. Available at: https://www.rpharms.com/about-us/news/details/RPS-in-Scotland-asks-for-further-support-and-recognition-for-pharmacy-teams (accessed April 2020)
[19] ITV. PPE from pandemic stockpile released to NHS and social care staff in Wales. 25 March 2020. Available at: https://www.itv.com/news/wales/2020-03-25/personal-protective-equipment-to-be-given-to-nhs-workers/ (accessed April 2020)
[20] NHS digital. Coronavirus (COVID-19). 2020. Available at: https://digital.nhs.uk/services/electronic-prescription-service (accessed April 2020)
[21] Pharmaceutical Services Negotiating Committee. Repeat dispensing/electronic Repeat Dispensing (eRD). Available at: https://psnc.org.uk/services-commissioning/essential-services/repeat-dispensing/ (accessed April 2020)
[22] Pharmaceutical Services Negotiating Committee. Post-dated prescriptions. Available at: https://psnc.org.uk/dispensing-supply/eps/dispensing-in-eps-release-2/post-dated-prescriptions-eps/ (accessed April 2020)
[23] Pharmacies urged to stay open seven days per week in the face of COVID-19. Pharm J online. 2020. doi: 10.1211/PJ.2020.20207824
[24] Pharmaceutical Services Negotiating Committee. Updated COVID-19 SOP and Opening Hours Flexibility: Statement from PSNC, CCA, NPA and AIM. 2020. Available at: https://psnc.org.uk/our-news/updated-covid-19-sop-and-opening-hours-flexibility-statement-from-psnc-cca-npa-and-aim/ (accessed April 2020)
[25] NHS England and NHS Improvement. Novel Coronavirus (COVID-19) standard operating procedure. Community Pharmacy. Available at: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/Novel-coronavirus-COVID-19-standard-operating-procedure-Community-Pharmacy-v2-published-22-March-2020.pdf (accessed April 2020)
[26] Pharmaceutical Services Negotiating Committee. COVID-19 Update: PQS, pharmacy services and payments. 2020. Available at: https://psnc.org.uk/our-news/covid-19-update-pqs-pharmacy-services-and-payments/ (accessed April 2020)
[27] National Pharmacy Association. Repackaging paracetamol during the coronavirus (COVID-19) pandemic. 2020. Available at: https://www.npa.co.uk/news-and-events/news-item/repackaging-paracetamol-during-the-coronavirus-covid-19-pandemic/ (accessed April 2020)
[28] General Pharmaceutical Council. Q&A: Coronavirus. 2020. Available at: https://www.pharmacyregulation.org/standards/guidance/questions-and-answers-coronavirus (accessed April 2020)
[29] Slawther E. Chemist + Druggist online. COVID-19: Wholesalers urge pharmacies to return tote boxes quickly. Available at: https://www.chemistanddruggist.co.uk/news/covid-19-wholesalers-urge-pharmacies-return-tote-boxes-quickly (accessed April 2020)
[30] Royal Pharmaceutical Society. Handwashing. Available at: https://www.rpharms.com/resources/pharmacy-guides/ams-portal/handwashing (accessed April 2020)
[31] UK Government. COVID-19: interim guidance for primary care. 2020. https://www.gov.uk/government/publications/wn-cov-guidance-for-primary-care/wn-cov-interim-guidance-for-primary-care#environmental-cleaning-following-a-possible-case (accessed April 2020)
[32] UK Government. COVID-19: guidance for supported living provision. 2020. Available at: https://www.gov.uk/government/publications/covid-19-residential-care-supported-living-and-home-care-guidance/covid-19-guidance-for-supported-living-provision (accessed April 2020)
[33] Deliveroo. You can now get contact-free deliveries. 2020. Available at: https://foodscene.deliveroo.co.uk/restaurant-profiles/introducing-contact-free-delivery.html (accessed April 2020)
[34] NHS England. Joint letter from Simon Stevens and Amanda Pritchard. 2020. Available at: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/20200317-NHS-COVID-letter-FINAL.pdf (accessed April 2020)
[35] Thomson Reuters Practical Law. Agency: definition. Available at: https://uk.practicallaw.thomsonreuters.com/1-107-6376?transitionType=Default&contextData=(sc.Default)&firstPage=true&bhcp=1 (accessed April 2020)
[36] Stewart K. Senior Editor Research & Learning at The Pharmaceutical Journal. Personal communication with PSNC. 2020.


