Shutterstock.com

Cancer learning ‘hub’
Pharmacists are playing an increasingly important role in supporting patients with cancer, working within multidisciplinary teams and improving outcomes. However, in a rapidly evolving field with numbers of new cancer medicines is increasing and the potential for adverse effects, it is now more important than ever for pharmacists to have a solid understanding of the principles of cancer biology, its diagnosis and approaches to treatment and prevention. This new collection of cancer content, brought to you in partnership with BeOne Medicines, provides access to educational resources that support professional development for improved patientRisk factors
Around 1 in 54 people will be diagnosed with a malignant melanoma during their lifetime, however, an individual’s risk of developing melanoma is dependent on a number of factors including age, genetics and exposure to risk factors. UV radiation from the sun and artificial UV radiation from sunbeds are the main potentially avoidable risk factors for skin cancer[4] . The main risk factors for melanoma skin cancer are discussed in more detail below.Age
As with most cancers, the risk of developing melanoma increases with age. Around 50% of all patients diagnosed with melanoma are over the age of 65[5] . However, younger people can develop melanoma; it is now the second most common cancer in people under 50 years of age and is the fifth most common cancer in people aged 15–24 years, accounting for 11% of the total number of cancers in this age group[3] .Skin type and colour
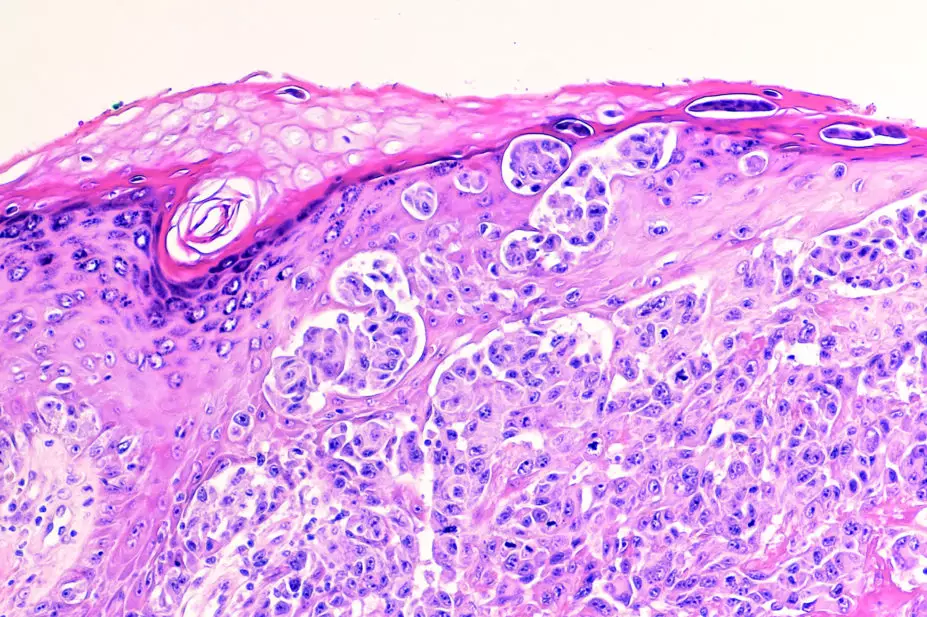
The Fitzpatrick skin type (see Figure 1) is a skin classification system used to determine a person’s skin type by their response to sun exposure in terms of the degree of burning and tanning[6] . Individuals who always burn, never tan and have pale white, blond or red hair, blue eyes and freckles are classed as skin type I, and have a higher risk of developing melanoma. Individuals at the end of the scale with darker skin, particularly those of Asian or African ethnicity, who never burn and always tan are classed as skin type VI, and have the lowest risk of developing melanoma. However, type VI patients may develop a specific type of melanoma, acral lentiginous melanoma (see Figure 2), which is found on the palms of hands, soles of feet or under finger or toe nails. 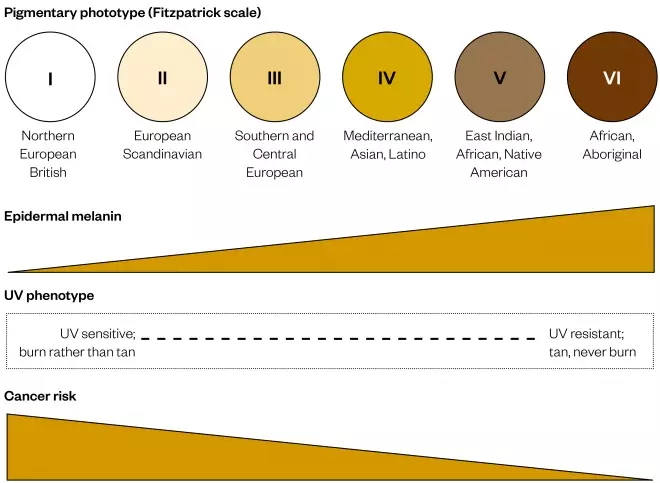
Figure 1: The Fitzpatrick skin type classification system
Six degrees of skin sensitivity to the sun predict the risk for developing melanoma. People at the lighter end have the highest risk, which goes down for people in the higher categories

Figure 2: Acral lentiginous melanoma
Source: Courtesy of Primary Care Dermatology Society (PCDS)
Acral lentiginous melanoma is a specific form of the disease that affects people with the darkest skin type, VI, who in general have the lowest risk of developing melanoma
Freckles and moles
Most people have 10–40 common moles on their body. Although common moles are not usually cancerous, people who have more than 50 common moles have a greater chance of developing melanoma[7] . Melanoma is 4–10 times higher in those with atypical naevi (large or unusually shaped moles) than those with common moles[8] . The risk of developing melanoma increases with number of moles (around a 2% increase in risk for every additional mole), and for individuals with more than 100 common moles, the risk is seven times higher than for those with few moles (0–5)[9] .UV light exposure
Exposure to UV light is the major environmental factor that increases risk of developing melanoma[10] . The World Health Organization has identified UV radiation as a proven human carcinogen[11] . UV light exposure can derive directly from the sun or artificial means (e.g. sunbeds). Solar UV light exposure is estimated to be the causative factor in 86% of malignant melanomas in the UK[12] and risk is more closely linked with intermittent high-intensity sunlight (e.g. holidaying in areas with strong sunlight) than with chronic exposure[13] . Around 100 cases of malignant melanoma deaths each year are accountable to sunbed use[14] .Sunburn
Although people who burn easily are more likely to have had sunburn as children, further sunburn events during adulthood also increase the chance of melanoma. The greater the total amount of sun exposure over a lifetime, the greater the chance of developing a melanoma, with risk more than double in people with a history of sunburn compared with those who have never been sunburnt[15] .Other risk factors
These include eye and hair colour, family history, genetic conditions, previous cancer, certain medical conditions (e.g. Parkinson’s, type II diabetes and congenital disorders), autoimmune diseases (e.g. Crohn’s disease and ulcerative colitis), exposure to specific infections (e.g. HIV), certain occupations (e.g. airline workers) and body characteristics including being taller than average and/or obese[3] . Further information on these risk factors can be found at Cancer Research UK.Tanning
Melanin is produced by melanocytes, cells located within the bottom layer of the epidermis, in a process called melanogenesis[16] . Melanin is a pigment and gives skin its colour. People who originate from warmer climates have darker skin that developed to protect them from UV exposure. For the same body region, people with fair and darker skin have roughly the same number of melanocytes (there is variation between different body regions), however, melanocytes in people with darker skin are more active and produce more melanin[17] . The main purpose of melanin is to protect the body from UV light exposure. A tan is actually a sign that the skin has been damaged and is trying to protect itself.Box 1: UVA and UVB
UV light reaches the earth from the sun in three wavelengths UVA, UVB and UVC. UVC does not penetrate the earth’s atmosphere and, as such, we are protected from its effects. UVA exposure is associated with skin ageing, as it affects elastin in the skin leading to wrinkles and sun-induced ageing, and can cause skin cancers. UVA penetrates skin deeper than UVB and can also pass through glass. UVB exposure is responsible for sunburn and is strongly linked to the development of melanomas[18] . More information can be found in the infographic ‘Science of sunscreen’.Sunscreens
There are two types of sunscreen: organic and inorganic[19] . Organic sunscreens contain filters that absorb UV light and convert it to infrared light, which is not damaging to skin. Inorganic sunscreens contain titanium dioxide or zinc oxide, which directly reflect the UV radiation. A useful way to think about the sunscreen types is to think of organic sunscreens as ‘sponges’ and inorganic sunscreens as ‘mirrors’. In the UK, sunscreens have both Sun Protection Factor (SPF) and UVA star systems. SPF relates to the ability of the sunscreen to protect the wearer from sunburn, therefore, primarily offering protection from UVB[19] . SPFs are rated on scales of 2–50+, with 2 offering the least protection and 50+ offering the most protection. SPF indicates the multiples of protection provided against burning compared with unprotected skin; for example, a SPF of 30 should enable a person to remain 30 times longer in the sun without burning than someone with unprotected skin. However, in practice, people do not apply sunscreen in sufficient quantities, therefore, protection is lower than anticipated. The UVA star system is rated from 0 to 5 stars and indicates the protection against UVA relative to protection against UVB. It is possible to have a high UVA star rating but low UVA protection because the SPF is low; it is a ratio between the two that determines the star rating[19] . The Royal Pharmaceutical Society (RPS) has called for clearer sunscreen labelling after the results of a public poll highlighted that only 8% of individuals knew that SPF rating referred only to protection from UVB radiation and not from UVA. The RPS has suggested that sunscreen manufacturers change the dual rating systems to one that combines both, based on a simple description of the total amount of sun protection offered: low, medium, high and very high protection[20] . Sunscreens come in multiple different formulations including creams, oils, sprays, sticks, moisturisers and make-up containing SPF, as well as once-a-day applications. However, not all formulations are created equal, with SPFs in moisturisers and make-up usually being at the lower end of the SPF scale (SPF 15), containing no UVA protection and unlikely to afford the sun protection that more typical sunscreens give[19] . Differences in formulation of the more typical sunscreens lead to differences in ease of application, the feel on the skin, whether the formulation has a drying effect on the skin and the cost of the product; all are important factors to take into account for individuals when selecting a sunscreen. More information can be found in the infographic ‘Science of sunscreen’.Evidence base for sunscreens
There has been scrutiny regarding the evidence base for sunscreens. Some have been shown to reflect or absorb UV light, however, whether this translates to a reduction in skin cancers has been controversial. A meta-analysis of observational case-control studies demonstrated no association between sunscreen use and the development of malignant melanoma[21] . However, in 2011, a randomised clinical study of 1,600 individuals demonstrated that regular sunscreen use reduced the incidence of melanoma by 50–73%[22] . The weight of evidence now resides with the use of sunscreens and UK health bodies including the National Institute for Health and Care Excellence (NICE), the health technology assessment body, and the British Association of Dermatologists (BAD), both advocate the use of sunscreens in conjunction with other sun protection measures[19] ,[23] . NICE recommends sunscreens must:- Provide at least SPF 15 to protect against UVB;
- Meet minimum UVA standards of protection (the label should have the letters ‘UVA’ in a circle logo)[23] .
Practical aspects for sunscreen selection and application
Pharmacists advising individuals on sunscreen should ensure that they have elicited enough information from them to help them make an informed choice. Important considerations include:Skin type
Patients with very fair skin that does not tan (type I skin) require sunscreens to be re-applied regularly throughout the day, as opposed to Asian or black skinned patients (type V–VI) who will only need sunscreen to be applied during extreme sun exposure[19] .Children
Sunscreen use in children aged under six months is not recommended as these children should not be exposed to direct sunlight. For children over six months, sunscreen should contain SPF15 or above and have good UVA protection (characterised by the UVA logo on the labelling)[23] .Activities
Water-based activities risk the removal of sunscreen through exposure to water and towel drying. The production of sweat through activities such as running or cycling can also remove sunscreens. Snow-based activities such as skiing and snowboarding require the use of sunscreen, despite the cool weather and scarcity of exposed skin. The amount of UV radiation that reaches earth increases with increase in altitude and snow reflects UV radiation more than water or sand. Water-resistant sunscreens are available. Water resistance is tested by the ability of a sunscreen to retain its sun protection properties following two 20 minute intervals (40 minutes total) of moderate activity in water. However, towel drying can remove 85% of the sunscreen, therefore, sunscreen should be re-applied when undertaking these activities; removal of sunscreen from the skin will render the sunscreen useless, no matter its SPF[19] .Application
Most people do not apply enough sunscreen and pharmacists should make patients aware that:- The amount of sunscreen for a body of an average adult to achieve the stated SPF is 35ml, or 6–8 teaspoons of lotion (this equates to 2mg/cm²). See Figure 3;
- If sunscreen is applied too thinly then protection is reduced;
- Areas such as the back and sides of the neck, temples and ears are commonly missed;
- Applying less sunscreen will reduce the protection to a higher degree than is proportionate — for example, only applying half the required amount can actually reduce the protection by as much as two-thirds;
- Sunscreen should be applied 15–30 minutes before going out in the sun to allow it to dry, and be re-applied shortly after heading outdoors to cover any missed patches. It should be applied in a sufficient layer;
- Sunscreen should be re-applied at least every two hours, and immediately after swimming, perspiring and towel drying, or if it has rubbed off[19] .
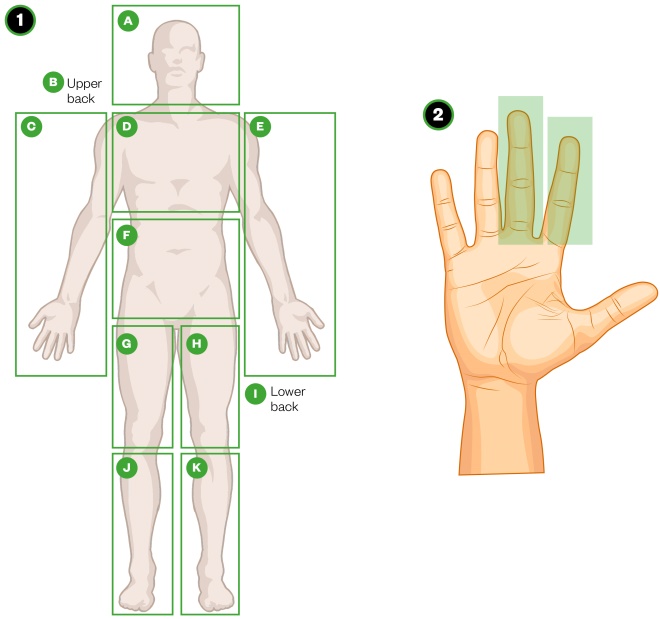
Figure 3: Sunscreen application
Source: The Sunscreen Smokescreen, Information Is Beautiful
1. Divide the body into 11 different areas, including the upper back and lower back. 2. Apply one or two fingers of sunscreen using the index and/or middle fingers. Using two fingers provides more optimal protection for around 2 hours.
Additional advice
- In the first instance, skin should be protected from strong sun exposure by wearing suitable clothing and seeking shade. Sunscreen is not an alternative to these measures and should be used in conjunction with them;
- Sunglasses with wraparound lenses or wide arms (to provide side protection) that have the CE mark should be worn to protect eyes;
- Spend time in the shade between 11am and 3pm when the UV radiation is at its highest levels;
- Keep babies and young children out of direct sunlight[23] .
World UV app
The World UV app has been developed in conjunction with BAD and the Met Office. It provides real-time information on daily UV levels from more than 10,000 locations around the world[19] .References
[1] Cancer Research UK. About melanoma. Available at: http://www.cancerresearchuk.org/about-cancer/melanoma/about (accessed June 2017)
[2] Cancer Research UK. Cancer incidence for common cancers. Available at: http://www.cancerresearchuk.org/health-professional/cancer-statistics/incidence/common-cancers-compared (accessed June 2017)
[3] Cancer Research UK. Skin cancer incidence statistics. Available at: http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/skin-cancer/incidence (accessed June 2017)
[4] Cancer Research UK. Risks and causes of melanoma. Available at: http://www.cancerresearchuk.org/about-cancer/melanoma/risks-causes (accessed June 2017)
[5] Office for National Statistics. Cancer registration statistics, England statistical bulletins. Available at: http://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/cancerregistrationstatisticsengland/previousReleases (accessed June 2017)
[6] Pathak MA, Jimbow K, Szabo G et al. Sunlight and melanin pigmentation. In Smith, K. C. (ed.): Photochemical and photobiological reviews, Plenum Press, New York, 1976:211–239.
[7] Tucker MA. Melanoma epidemiology. Hematol Oncol Clin North Am 2009;23(3):383–395. doi: 10.1016/j.hoc.2009.03.010
[8] Gandini S, Sera F, Cattaruzza MS et al. Meta-analysis of risk factors for cutaneous melanoma: I. Common and atypical naevi. Eur J Cancer 2005;41:28–44. doi: 10.1016/j.ejca.2004.10.015
[9] Olsen CM, Carroll HJ & Whiteman DC. Estimating the attributable fraction for cancer: A meta-analysis of nevi and melanoma. Cancer Prev Res (Phila) 2010;3(2):233–245. doi: 10.1158/1940-6207.CAPR-09-0108
[10] International Agency for Research on Cancer. Solar and ultraviolet radiation (Vol 55). Monographs on the evaluation of carcinogenic risks to humans. Lyon: IARCPress;1992. Available at: http://monographs.iarc.fr/ENG/Monographs/vol55/ (accessed June 2017)
[11] World Health Organization. Cancer prevention. Available at: http://www.who.int/cancer/prevention/en/ (accessed June 2017)
[12] Parkin DM, Mesher D & Sasieni P. 13. Cancers attributable to solar (ultraviolet) radiation exposure in the UK in 2010. Br J Cancer 2011;105 Suppl 2:S66–S69. doi: 10.1038/bjc.2011.486
[13] Gandini S, Sera F, Cattaruzza MS et al. Meta-analysis of risk factors for cutaneous melanoma: II. Sun exposure. Eur J Cancer 2005;41:45–60. doi: 10.1016/j.ejca.2004.10.016
[14] Diffey BL. A quantitative estimate of melanoma mortality from ultraviolet A sunbed use in the UK. Br J Dermatol 2003;149:578–581. doi: 10.1046/j.1365-2133.2003.05420.x
[15] Elwood JM & Jopson J. Melanoma and sun exposure: an overview of published studies.Int J Cancer 1997;73:198–203. doi: 10.1002/(SICI)1097-0215(19971009)73:2<198::AID-IJC6>3.0.CO;2-R
[16] Cichorek M, Wachulska M, Stasiewicz A et al. Skin melanocytes: biology and development. Postep Dermatol Allergol 2013;30(1):30–41. doi: 10.5114/pdia.2013.33376
[17] Barsh GS. What controls variation in human skin color? PLoS Biol 2003;1(1):e27. doi: 10.1371/journal.pbio.0000027
[18] D’Orazio J, Jarrett S, Amaro-Ortiz A et al. UV Radiation and the skin. Int J Mol Sci 2013;14(6):12222–12248. doi: 10.3390/ijms140612222
[19] British Association of Dermatologists. Sunscreen fact sheet. How do sunscreens work? Available at: http://www.bad.org.uk/for-the-public/skin-cancer/sunscreen-fact-sheet#how-do-sunscreens-work (accessed June 2017)
[20] Make sunscreen protection rating clearer, urges pharmacist organisation. Pharm J 2015;295(7870). doi: 10.1211/PJ.2015.20068834
[21] Diffey BL. Sunscreens as a preventative measure in melanoma: an evidence-based approach or the precautionary principle? Br J Dermatol 2009;161(Suppl. 3):25–27. doi: 10.1111/j.1365-2133.2009.09445.x
[22] Green AC, Williams GM, Logan V & Strutton GM. Reduced melanoma after regular sunscreen use: randomized trial follow-up. J Clin Oncol 2011;29(3):257–263. doi: 10.1200/JCO.2010.28.7078
[23] National Institute for Health and Care Excellence (NICE). Sunlight exposure: risks and benefits. Available at: https://www.nice.org.uk/guidance/ng34/chapter/1-Recommendations (accessed June 2017)
[24] Sunscreen SPFs: clear as daylight? Drug and Therapeutics Bulletin 2011;49:61.