
JL / The Pharmaceutical Journal
Meningitis is the second leading infection-related cause of death in children in the world, second only to pneumonia[1]
. It is responsible for more deaths than malaria, AIDS, measles and tetanus combined[1]
. The disease is more prevalent in children under the age of four years and in teenagers. In England, there has been a decline in confirmed cases of invasive meningococcal disease over the past two decades, from 2,595 cases in 1999/2000 to 755 cases in 2017/2018, which is a small increase from the 748 cases reported in 2016 and 2017[2]
.
Pharmacists have a vital role in raising awareness of the signs and symptoms of meningitis, while also maximising the benefit of the national immunisation programme to reduce the incidence of the disease. This article will cover initial management options, with a focus on children and neonates.
Causes
Meningitis — inflammation of the membranes covering the brain and spinal cord (meninges) — can be caused by viruses, bacteria or fungi.
Meningococcal disease encompasses meningococcal septicaemia (25% of cases), meningococcal meningitis (15% of cases) or a combination of the two (60% of cases)[3]
. Up to 95% of meningitis in the UK is aseptic, where there is no growth on cerebrospinal fluid (CSF) culture, usually with a viral aetiology (e.g. enteroviruses)[3]
.
Bacterial meningitis is most commonly caused by Neisseria meningitidis (also known as meningococcus), although the main pathogens alter with age. As such, N. meningitidis, Streptococcus pneumoniae (also known as pneumococcus) and Haemophilus influenzae type b are the leading causes of meningitis in children older than three months; however, Streptococcus agalactiae, Escherichia coli, S. pneumoniae and Listeria monocytogenes are more common in children younger than three months[3]
.
The bacteria that cause meningitis are very common — they are present in the nasopharynx in around one in ten people who may not ever show any symptoms of disease. The reasons why some people develop meningitis while others do not are not yet fully understood. However, it is thought that genetic variations in the genes for Factor H and Factor H-related proteins may have a role to play[4]
. These proteins regulate a part of the body’s immune system called the complement system, which recognises and kills invading bacteria.
Risk factors
In general, young children are at the highest risk of bacterial meningitis and septicaemia, but other age groups, including older people, can also be vulnerable to specific types. One study found that meningococcal meningitis was less frequent in older patients, whereas pneumococcal, listerial and meningitis of unknown origin were more frequent[3],
[5]
. People with low immunity, for example, those with HIV or those having chemotherapy treatment for cancer, may also be at an increased risk.
Individual countries show seasonal patterns of bacterial meningitis. For instance, increased cases have been observed between the months of December and March in the United States, France and the UK[6]
. There is also evidence that mass gatherings and exposure to cigarette and wood smoke can make people more susceptible to certain causes of meningitis and septicaemia, potentially from interference with mucosal immunity[7]
.
Depending on the cause, cases of meningitis may be isolated. However, those who have been in close contact with someone with bacterial meningitis may be at increased risk of disease.
Pathophysiology
Infection occurs through transmission of contaminated respiratory droplets or saliva. Pili on the bacterial surface are thought to disrupt endothelial cell junctions in the blood–brain barrier, allowing the pathogens to penetrate it[8]
. Once they have entered the subarachnoid space (the area of the brain between the arachnoid membrane and the pia mater), the pathogens replicate rapidly. This causes the production of several inflammatory mediators, including lymphocytes and inflammatory cytokines, as well as local immunoglobulin production by plasma cells. This enhances the influx of leukocytes into the CSF, which releases toxic substances that contribute to the production of cyctotoxic oedema and increased intracranial pressure. It is this process that can contribute to neurological damage and even death[9],[10]
.
Signs, symptoms and immediate management
Symptoms typically occur within 3–7 days after transmission[3]
. Early, non-Âspecific symptoms of meningitis include:
- Irritability;
- Ill appearance;
- Lethargy;
- Refusing food/drink;
- Headache;
- Other aches and respiratory symptoms;
- Vomiting/nausea;
- Fever.
Healthcare professionals should be aware that classic signs of meningitis that include neck stiffness, bulging fontanelle and high-pitched cry are often absent in infants with bacterial meningitis[3],[11]
. Less common early symptoms include shivering, diarrhoea, abdominal pain and distention, coryza and other ear, nose and throat symptoms[3]
.
General features of meningitis include a nonÂ-blanching rash that can appear anywhere on the body, altered mental state, shock, unconsciousness and toxic or moribund state. If a patient presents with these symptoms, the glass test (also known as the ‘Tumbler test’; see Figure 1) may be used to aid diagnosis, where the side of a clear glass should be firmly pressed against the rash; if it does not fade under pressure, the patient may have septicaemia and needs urgent medical attention (see Figure 2)[3],[12]
. However, it should be noted that the National Institute for Health and Care Excellence’s Clinical Knowledge Summary states that the glass test should not be used solely for diagnosing bacterial meningitis and meningococcal septicaemia[13]
.

Figure 1: Glass or ‘tumbler’ test
Source: Alamy Stock Photo / Mediscan
A rash that does not fade under pressure is a sign of meningococcal septicaemeia. However, this test should not be used solely in diagnosis.
The classic rash associated with meningitis usually looks like small, red pin pricks that spreads quickly over the body and turns into red or purple blotches. However, a rash is not always present with meningitis and may be less visible in darker skin tones. It is, therefore, important to also check the soles of the feet, palms of the hands and eyelids in the patient with suspected meningitis[3]
.
Furthermore, if the patient is a child or young person, it is important for healthcare professionals to consider other non-specific features of their presentation, such as the level of parental or carer concern (particularly compared with previous illness in the child or young person or their family), how quickly the illness is progressing, and clinical judgement of the overall severity of the illness[3]
.
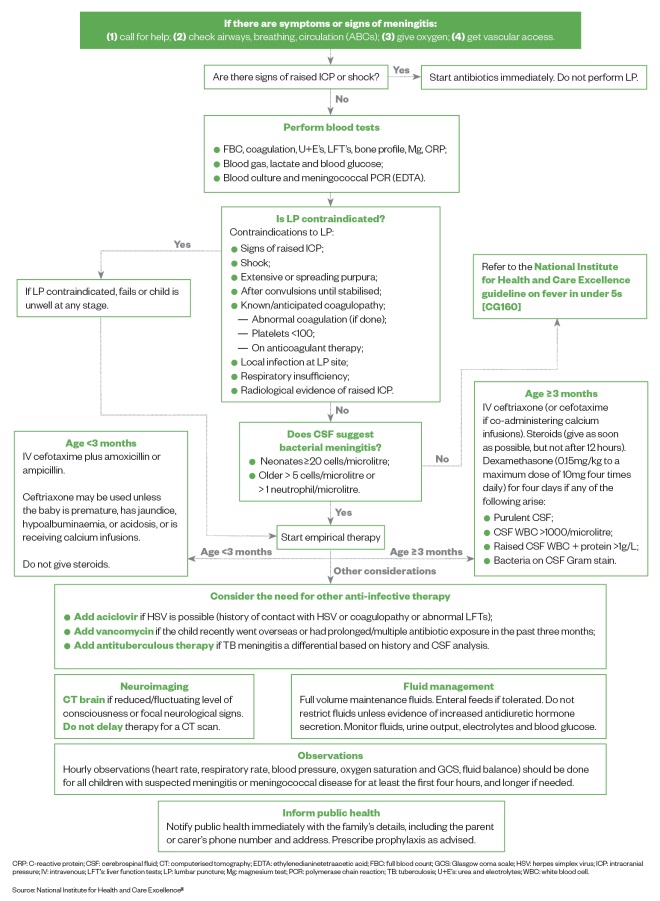
Figure 2: Immediate management of suspected meningitis in children and neonates
Source: National Institute for Health and Care Excellence
[3]
CRP: C-reactive protein; CSF: cerebrospinal fluid; CT: computerised tomography; EDTA: ethylenedianinetetraacetic acid; FBC: full blood count; GCS: Glasgow coma scale; HSV: herpes simplex virus; ICP: intracranial pressure; IV: intravenous; LFT’s: liver function tests; LP: lumbar puncture; Mg: magnesium test; PCR: polymerase chain reaction; TB: tuberculosis; U+E’s: urea and electrolytes; WBC: white blood cell.
Prevention and vaccination
As meningitis can be caused by several different pathogens, there are several vaccinations available that can offer some protection against the disease (see Table)[10]
.
| Vaccine | Protection | Childhood immunisation schedule | Other patient groups |
|---|---|---|---|
| Meningitis B vaccine | This vaccine offers protection against meningococcal group B bacteria — a common cause of meningitis in young children in the UK | 8 weeks 16 weeks 1 year | N/A |
| 6-in-1 vaccine (DTaP/IPV/Hib/Hep B) | This vaccine offers protection against:
| 8 weeks 12 weeks 16 weeks | N/A |
| Pneumococcal vaccine | This vaccine offers protection against serious infections caused by pneumococcal bacteria, including meningitis | 8 weeks 16 weeks 1 year |
|
| Hib/Meningitis C vaccine | This vaccine offers protection against meningococcal group C bacteria that can cause meningitis | 1 year |
|
| MMR vaccine | This vaccine offers protection against measles, mumps and rubella. Meningitis can sometimes occur as a complication of these infections | 1 year 3 years and 4 months |
|
| ACWY: the meningococcal strains A, C, W and Y; DTaP: diphtheria, tetanus and pertussis vaccine; Hep B: heptatitis B; Hib: Haemophilus influenzae type b; IPV: inactivated poliovirus vaccine; MMR: measles, mumps and rubella | |||
Case studies
Several case studies show how assessment and treatment of meningitis varies by patient. All patients, events and incidents in these case studies are fictitious and should only be used as examples in the clinical setting.
Case study 1: a toddler with mild meningitis
Eva is a three-year-old girl who is on holiday with her grandparents. Eva is unusually tired and is complaining that her legs are aching. This morning, Eva’s grandparents noticed a very small purple rash on her leg, and so they have to come to the pharmacy for advice. Eva has no fever or any other symptoms, but her grandmother has a cold sore.
Assessment and diagnosis
The rash does not fade under pressure when a glass is pressed against it.
Petechiae and purpura are significantly more common with invasive meningococcal infection than with pneumococcal meningitis, which rarely presents with a rash[13]
. However, although the glass test is widely promoted in patient information leaflets, the National Institute for Health and Care Excellence (NICE) has found no evidence on its use. The test is not promoted in the NICE guidelines. Consequently, the glass test should not be used as the only test for diagnosing the condition[12]
. Public Health England is also informed that Eva may have meningitis, and 999 is called.
Treatment options
On arrival at hospital, Eva is showing signs of shock — she is tachycardic with increased drowsiness and cold peripheries. After having initial tests, she is treated for shock with a fluid bolus of 20mL/kg sodium chloride 0.9% over 10 minutes. A lumbar puncture is contraindicated in shock and, therefore, Eva is empirically started on intravenous (IV) ceftriaxone and steroids. She is also started on IV aciclovir, owing to her history of contact with the herpes simplex virus.
Advice and recommendations
Eva is treated with antibiotics for ten days and her grandparents are both prescribed rifampicin as chemoprophylaxis. Antibiotic prophylaxis should be given as soon as possible (ideally within 24 hours) after the diagnosis of the index case[12]
.
Case study 2: a baby with meningitis
Katherine is a mother of two young children who comes into the pharmacy and asks for advice. She has a young baby, Jacob, who is six weeks old and Esmé who is four years old. Jacob has a blocked nose and fever. Katherine explains that Esmé had gastroenteritis with cold symptoms and fever last week, but no rash. Katherine is worried about Jacob and asks for advice.
Assessment and diagnosis
Katherine brings her children into the consultation room for further assessment. Jacob has been more unsettled than usual and does not want to feed as much as normal. Upon examination, Jacob has a rash on his stomach and back, which his mother says was not present this morning. His rash looks like red blotches and does not fade with the glass test. Owing to his age, Jacob is too young to have received any vaccinations.
It is important to remain calm and inform Katherine that you think Jacob may have meningitis, as he has the characteristic rash, as well as other known symptoms. Jacob needs to be taken to hospital for emergency assessment and an ambulance is called.
Treatment options
On arrival at the hospital, Jacob has blood tests taken and a lumbar puncture. He is started on intravenous (IV) cefotaxime with amoxicillin (if he was three months or older, IV ceftriaxone would be administered) with full-volume maintenance fluids and enteral feeds as tolerated[3]
. Corticosteroids must not be used in children aged younger than three months with suspected or confirmed bacterial meningitis.
Jacob has hourly observations initially for heart rate, blood pressure, respiratory rate, oxygen saturation, fluid balance and Glasgow Coma Scale (GCS). The GCS is a neurological scale used to describe the level of consciousness in a person following a traumatic brain injury — the lower the number, the more severe the brain injury. Public Health England is also informed that Jacob may have meningitis.
In children younger than three months, ceftriaxone may be used as an alternative to cefotaxime (with or without ampicillin or amoxicillin); however, it should not be used in premature babies or in babies with jaundice, hypoalbuminaemia or acidosis, as it may exacerbate hyperbilirubinaemia[3]
.
The microbiology consultant calls the ward to confirm that Jacob has Group B streptococcal meningitis. As per the National Institute for Health and Care Excellence’s guidelines, Jacob will need treating with IV cefotaxime for at least 14 days[3]
.
Advice and recommendations
Before discharge, Katherine is given the contact details of several patient support organisations, including meningitis charities that can offer support and written information to signpost her to further help. Jacob has an audiology appointment booked in two weeks and will be seen by a paediatrician after this. At this appointment, the following morbidities will be considered:
- Hearing loss;
- Orthopaedic complications;
- Skin complications (including scarring from necrosis);
- Psychosocial problems;
- Neurological and developmental problems;
- Kidney failure.
Outcome of the advice
Jacob makes a full recovery from his meningitis with no lasting effects.
Case study 3: an adult with suspected meningitis
Jane is a paediatric haematology nurse who comes into the pharmacy asking to buy paracetamol. She says she has a terrible headache and upset stomach. She seems confused and disorientated; talking to her further highlights that something is not right.
Jane explains that she has not felt well since last night and has spent most of the day in bed, as she feels like she has no energy. However, some of what Jane also says does not make sense, and she is finding it hard to follow the conversation. She has no fever or rash.
Assessment and diagnosis
Vomiting, severe headache and confusion are all symptoms of meningitis. Using a symptoms checker, such as the one by the Meningitis Research Foundation, to help with decision making.
Upon further questioning, it is clear that Jane must go to a hospital immediately and an ambulance is called. Jane presented with confusion and disorientation, which might indicate a stroke; however, bacterial meningitis can cause stroke.
Treatment options
When the paramedics arrive at the pharmacy, they find Jane has a Glasgow Coma Scale of 4/15. Once Jane arrives in hospital, they follow the stroke pathway, but she is now also febrile. Jane has a lumbar puncture and the results show she has bacterial meningitis. She also has a CT scan that shows an infarct on her right temporal lobe. Jane is treated in hospital with antibiotics and steroids, and eventually discharged to go home after three weeks.
Jane was working in the paediatric intensive care unit the week preceding the symptoms. She was looking after a child with Haemophilus influenzae type b (Hib). The patient was in a neutral pressure side room with a positive pressure lobby — this is an infection control measure to prevent the spread of microbial contaminants outside the patient’s side room. The lobby had been used to store an apheresis machine; however, the door between the side room and lobby had been left open, inadvertently leading to the exposure of Hib.
Outcome of the advice
Although Jane has now fully recovered, she has to wear glasses owing to damage to her optical nerve. She also has tinnitus and occasionally suffers from severe headaches.
Recovering from meningitis/complications
Some of the most common complications associated with meningitis are[10]
:
- Hearing loss, which may be partial or total — people who have had meningitis will usually have a hearing test after a few weeks to check for any problems;
- Recurrent seizures;
- Problems with memory and concentration;
- Problems with coordination, movement and balance;
- Learning difficulties and behavioural problems;
- Vision loss, which may be partial or total;
- Loss of limbs — amputation is sometimes necessary to stop the infection spreading through the body and remove damaged tissue;
- Bone and joint problems, such as arthritis;
- Kidney problems.
Overall, it is estimated that up to one in every ten cases of bacterial meningitis is fatal.
References
[1] UNICEF, WHO, World Bank Group & United Nations. Levels and Trends in Child Mortality Report. 2017. Available at: https://www.unicef.org/publications/index_101071.html (accessed June 2019)
[2] Public Health England. Invasive meningococcal disease in England: annual laboratory confirmed reports for epidemiological year 2017 to 2018. 2018. Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/751821/hpr3818_IMD.pdf (accessed June 2019)
[3] National Institute for Health and Care Excellence. Meningitis (bacterial) and meningococcal septicaemia in under 16s: recognition, diagnosis and management. Clinical guideline [CG102]. 2015. Available at: https://www.nice.org.uk/guidance/cg102 (accessed June 2019)
[4] Davila S, Wright VJ, Khor CC et al. Genome-wide association study identifies variants in the CFH region associated with host susceptibility to meningococcal disease.Nat Genet 2010;42(9):772–776. doi: 10.1038/ng.640
[5] Domingo P, Pomar V, de Benito N & Coll P. The spectrum of acute bacterial meningitis in elderly patients. BMC Infect Dis 2013;13:108. doi: 10.1186/1471-2334-13-108
[6] Paireau J, Chen A, Broutin H et al. Seasonal dynamics of bacterial meningitis: a time-series analysis. Lancet Glob Health 2016;4(6):e370–e377. doi: 10.1016/S2214-109X(16)30064-X
[7] Cooper LV, Robson A, Trotter CL et al. Risk factors for acquisition of meningococcal carriage in the African meningitis belt. Trop Med Int Health 2019;24(4):392–400. doi: 10.1111/tmi.13203
[8] Kolappan S, Coureuil M, Yu X et al. Structure of the Neisseria meningitidis type IV pilus. Nat Commun 2016;7:13015. doi: 10.1038/ncomms13015
[9] Tunkel AR & Scheld WM. Pathogenesis and pathophysiology of bacterial meningitis. Clin Microbiol Rev 1993;6(2):118–136. doi: 10.1128/CMR.6.2.118
[10] Sáez-Llorens X & McCracken GH Jr. Bacterial meningitis in children. Lancet 2003;361(9375):2139–2148. doi: 10.1016/S0140-6736(03)13693-8
[11] NHS Choices. Meningitis. 2019. Available at: https://www.nhs.uk/conditions/meningitis (accessed June 2019)
[12] Baines P, Reilly N & Gill A. Paediatric meningitis: clinical features and diagnosis. Clin Pharm 2009;1:307–310. URI: 10971150
[13] The National Institute for Health and Care Excellence. Clinical Knowledge Summaries: meningitis — bacterial meningitis and meningococcal disease. 2019. Available at: https://cks.nice.org.uk/meningitis-bacterial-meningitis-and-meningococcal-disease (accessed June 2019)
[14] NHS Choices. Pneumococcal vaccination. 2019. https://www.nhs.uk/conditions/vaccinations/pneumococcal-vaccination (accessed June 2019)
[15] Cooper LV, Robson A, Trotter C et al. Risk factors for acquisition of meningococcal carriage in the African meningitis belt. Trop Med Int Health 2019;24(4):392–400. doi: 10.1111/tmi.13203
You might also be interested in…

Case-based learning: insect bites and stings

Management of cold and flu symptoms
