This content was published in 2006. We do not recommend that you take any clinical decisions based on this information without first ensuring you have checked the latest guidance.
The varicella zoster (VZ) virus is highly infectious and causes the common childhood infection chickenpox (varicella). After recovery from a primary chickenpox infection the virus lays dormant in the sensory nervous system to reemerge as shingles (herpes zoster) in 20 per cent of adults over the age of 60 years.
Chickenpox
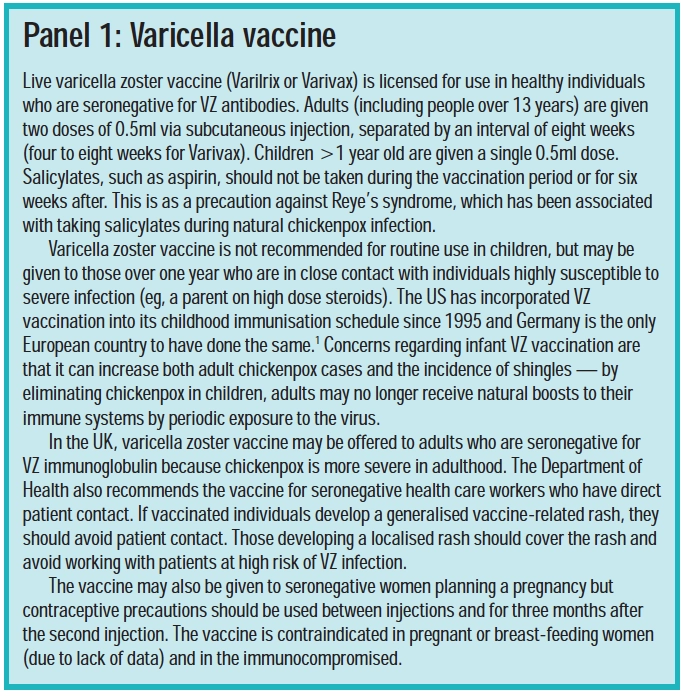
In the UK and other temperate climates without a childhood vaccination programme (see Panel 1), chickenpox predominantly occurs in pre-school and early school years and 90 per cent of individuals have had chicken pox by young adulthood. Outbreaks of chickenpox are usually widespread, with peak incidences in winter and early spring. In the tropics the pattern of infection is different — only 50 per cent of young adults have immunity to the disease, therefore proportionately more cases occur in adulthood. The reason for this is not known but this should be borne in mind by pharmacists practising in areas of the UK where significant sections of the population are originally from tropical regions.
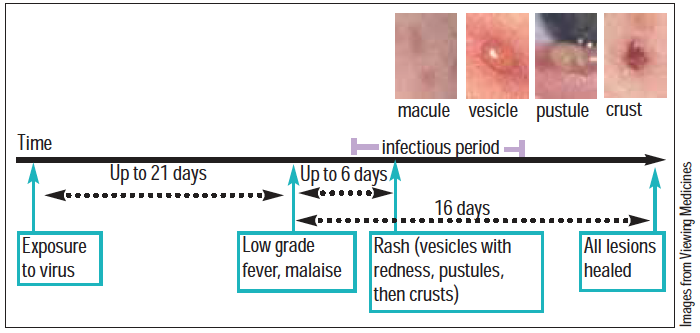
The first symptoms of infection are usually a low-grade fever, malaise and, sometimes, mild influenza-like symptoms, including adry cough. These symptoms are followed by a rash up to six days later and over the subsequent three to five days, crops of small red spots (macules) appear. This clustering and the location of the spots usually makes diagnosis clear — they commonly start behind the ears, on the face or on the trunk (often under the arms) and then spread further, although they tend to be sparse on the limbs.
In some cases, the rash involves the mucous membranes of the mouth (lesions burst to leave painful ulcers), nose and vulva. Within a few hours, the spots turn into fluid-filled blisters about 3mm in diameter (vesicles), then develop into pustules (spots containing pus) and crust over before healing.
At the peak of the illness there are lesions at all stages of development, from new spots through to crusts. The lesions are intensely itchy at all stages. Time for total healing of alllesions is around 16 days.
The number of spots varies widely. Some patients may have only one or two and the illness may pass undetected whereas others are covered in spots. Sometimes it is not clinically obvious that a child has contracted chickenpox, but if one person in a house has chickenpox then other previously uninfected household members have a greater than 90 per cent chance of contracting the disease. Infection with VZ usually confers lifelong immunity and it is rare to have more than one episode of chickenpox.
Transmission of VZ is via expired airborne droplets, direct contact with vesicle fluid or indirect contact with infected clothes, bedding or other articles. The incubation period (the time from acquisition of the virus to emergence of symptoms) is commonly 10–14 days, but may be as long as 21 days. However, people are only infectious from about 48 hours before and until five to six days after appearance of the first spots. Children should be kept away from school during this time, according to nursery and school policies.
Conditions that might be confused with chickenpox include herpes simplex, shingles (see below), impetigo, urticaria, scabies, Coxsackie virus infection and adverse drug reactions.
Identify knowledge gaps
- What are the possible complications of chickenpox?
- What should a pregnant woman with no history of chickenpox do if she comes into contact with the varicella zoster virus?
- What is postherpetic neuralgia and how is it managed?
Before reading on, think about how this article may help you to do your job better. The Royal Pharmaceutical Society’s areas of competence for pharmacists are listed in “Plan and record”, (available at: www.rpsgb.org/education). This article relates to “common disease states”.
Management
Management of symptoms is all that is required in immunocompetent people. Paracetamol and ibuprofen will reduce the flu-like symptoms and fever. Antivirals are not recommended for healthy adults and children in the absence of complications: there is evidence of only minor benefit (symptom reduction by one day if started within 24 hours of rash onset and no reduction in complications).
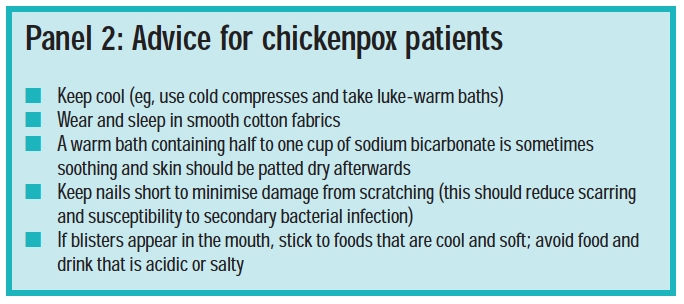
Itching
The sedating antihistamine chlorphenamine is specifically licensed for itching in chickenpox in those over the age of one year and can reduce distress and sleeplessness. Hydroxyzine is an alternative and is licensed for use in children over six months. Itching may also be eased with crotamiton, which has a helpful soothing effect. Available in a cream or lotion, it cannot be sold for use on those under three years (although it is prescribable for babies from one month) or by pregnant women. It is applied two or three times daily but the skin should not be broken or inflamed, so care must be taken when applying the product to scratched lesions.

Calamine preparations are often used in chickenpox although little benefit is seen in most people. They cause counter-irritation and evaporation gives a cooling effect. Formulation options are a water-based cream or lotion or an oil-based lotion. The latter contains peanut oil and lanolin, so caution should be exercised with respect to allergy. Choice of formulation is made according to personal preference and the extent of the rash. The cream or lotion is applied liberally to affected areas with clean cotton wool. Calamine can stain clothing.
Further advice pharmacists can give islisted in Panel 2.
Complications
Chickenpox is usually mild and self-limiting but complications can occur, especially in the immunocompromised. The disease tends to be mild in young children but is considerably unpleasant in adults, when complications are more likely.
The most common complication of chickenpox is bacterial skin infection. This occurs in 5–10 per cent of cases and requires topical or oral antibiotics, depending on the extent and severity of the infection (oral agents are flucloxacillin or erythromycin). Group A Streptococcus pyogenes and Staphylococcus aureus are common infecting organisms. Otitis media is a common complication in children.
In adults, varicella pneumonia (appearing three to four days after the rash and characterised by wheezing and rapid breathing) is the most common serious complication causing 20–30 hospital admissions per 10,000 adults.2 The likelihood of scarring (round, deep, punched-out lesions or pock marks) also increases with age. Other serious complications include:
- Acute cerebellar ataxia (sudden onset of muscle incoordination, which can occur after a viral infection is seen in 1 in 4,000 children under 15 years with chickenpox)
- Encephalitis
Overall, chickenpox causes about 25 deaths annually in England and Wales.
Pharmacists can play a health promotion role by giving advice about infectivity. People who are infected should be advised to avoid contact with pregnant women and those who are immunocompromised.
Pregnancy
Primary infection with VZ can be severe in pregnancy and can threaten fetal and neonatal health. It can cause maternal mortality or severe morbidity, namely pneumonia (in 10 per cent of cases), hepatitis and encephalitis and can cause fetal varicella syndrome or chickenpox in the newborn baby.3 Infection in young babies can be serious because their immune systems are weak.
Women planning a pregnancy who believe they have not had chickenpox should be advised to visit their GP for a blood test to assess their immunity. If the test reveals a woman has no VZ antibodies she can choose to be vaccinated with the live VZ vaccine (see Panel 1). Women from tropical or subtropical areas should have their immune status checked because they are more likely to be seronegative for VZ antibodies.
Pregnant women commonly come into contact with VZ (especially if they already have children) but more than 90 per cent of women are seropositive for VZ antibodies, so contact is not usually a cause for concern. However, pregnant women who have not or cannot remember having had chickenpox, should have their immune status assessed ift hey have significant contact with the virus. Significant contact has been defined as face-to-face conversation for five minutes, over 15 minutes in the same room, or living in the same household.3 About 80–90 per cent of these women will be reassured by a seropositive result but if the blood test reveals that the woman is seronegative for VZ antibodies and she does not show clinical signs of chickenpox, she should be given VZ immunoglobulin as soon as possible and within 10 days of contact. Administration of the immunoglobulin may not prevent chickenpox but it will lessen the severity of the infection and its risks.
If a pregnant woman shows clinical signs of chickenpox she should seek medical advice and avoid contact with other pregnant women and neonates. Aciclovir is recommended by the Royal College of Obstetricians and Gynaecologists for women with chickenpox who are more than 20 weeks pregnant if started within 24 hours of rash onset. No adverse fetal or neonatal effects associated with aciclovir in pregnancy have been reported.
The implications of maternal VZ infection for the fetus depend on the gestation period. Before 20 weeks, fetal varicella syndrome maycause skin scarring, eye defects, limb hypoplasia and neurological abnormalities in 1–2 percent of cases. Infection between 20 and 36 weeks’ gestation appears not to affect the fetus, but may lead to shingles in the first few years of life.
If clinical signs of chickenpox (the rash) occurs one to four weeks before delivery, up to 50 per cent of babies are infected and approximately a quarter develop chickenpox. Infection is particularly severe if maternal chickenpox occurs between four days before and two days after delivery, because the cord blood level of VZ antibodies will not have reached a sufficient level to protect the neonate. The neonate’s own immune system will be immature so he or she will need to be given VZ immunoglobulins and, if signs of infection are seen, intravenous aciclovir.
Immunocompromised individuals
HIV-infected individuals, patients with cancer, transplant recipients, people who have had radiotherapy or chemotherapy within six months and those taking, or having recently taken, systemic corticosteroids are at high risk of severe disseminated chickenpox (where other organs in addition to the skin are affected) and its complications. Chickenpox in these individuals can result in death so specialist attention is urgently needed if VZ contact is suspected.
Post-exposure prophylaxis with VZ immunoglobulin lessens severity if not preventing disease, and should be given as early as possible following contact. Treatment of chickenpox in immunocompromised individuals is with aciclovir. This is usually given intravenously, but oral aciclovir may be prescribed to those considered mildly immunocompromised (eg, patients taking low dose corticosteroids).
Shingles
After the first infection, VZ remains dormantin the dorsal root ganglia of the spinal cord. It is kept in check by the host’s immune system, but if reactivated (eg, due to a decrease in cell-mediated immunity) it travels along the sensory nerve to affect one or more dermatomes (area of the skin innervated by fibres from a single spinal nerve). Pain, tingling, itching or burning (or all of these) may occur over the affected dermatome for up to a week (commonly two or three days) before appearance of the shingles rash — a prodromal phase. There may also be systemic symptoms such as fever and malaise.

The rash is almost always unilateral and usually only one dermatome is affected (ie, the rash is localised). The abdomen, chest, face (above and below one eye) and neck are the most common sites — thoracic dermatomes are affected in 56 per cent of shingles cases, followed by cranial (13 per cent, usually the ophthalmic division), lumbar (13 per cent) and cervical (11 per cent) dermatomes.4 Lesions are similar to those in chickenpox: starting as erythematous and maculopapular, developing into vesicles and, eventually, crusting over. New lesions form over three to five days and fully heal over two to four weeks. Disseminated herpes zoster (where the virus affects other organs of the body) can occur in the immunocompromised.
Viral reactivation may be caused by normal ageing (50 per cent of people over 80 years are affected), disease, physical or emotional stress, fatigue, poor nutrition or chemo- or radio-therapy. A double-blind, placebo-controlled trial investigating the effect of vaccination with live varicella zoster vaccine on incidence and severity of shingles in the older population gave interesting results. In the study, 38,546 adults of 60 years or older were given the vaccine and followed-up for three years. Findings were that the vaccine reduced incidence of shingles by 51 per cent and reduced incidence of postherpetic neuralgia (see below) in those who had been given the vaccine but still developed shingles, by 67 percent.5 Perhaps, therefore, vaccinations should be considered for decreasing the incidence and impact of this common and often debilitating illness of older age.
Shingles is contagious by direct contact andcan cause chickenpox. However, if the rash is covered, transmission is unlikely. Patients should be advised to avoid sharing towels and to abstain from swimming and contact sports. It is unusual for immunocompetent individuals to develop shingles more than once (<5 percent).
Management
Nerve pain is the most troublesome complaint in shingles and can be severe. It is managed using a stepwise approach, starting with paracetamol. A weak opioid, such as codeine, 30–60mg up to four times daily, may be added. Occasionally, it is necessary touse a strong opioid, such as morphine. Icepacks may also help.
Antiviral treatment is recommended for:
- People over 50 years
- People with severe acute pain and an extensive rash
- People who are immunocompromised
- People with ophthalmic involvement
- People with Ramsay-Hunt Syndrome
- People with atopic eczema
However, antivirals should be discussed with and offered to the under 50s as well. Aciclovir (800mg, five times a day for seven days for those over 16 years) is the drug of choice and should be started within 72 hours of the onset of the rash. Where compliance is an issue, the more expensive valaciclovir or famciclovir may be prescribed.
Good skin hygiene is important to reduce the risk of secondary bacterial infection.

Complications
The most common complication of shingles is postherpetic neuralgia (nerve pain persisting after the rash has healed). This can be a steady burning, aching pain, a jabbing pain, or a combination and may be triggered by innocuous stimuli such as clothing moving against the skin.
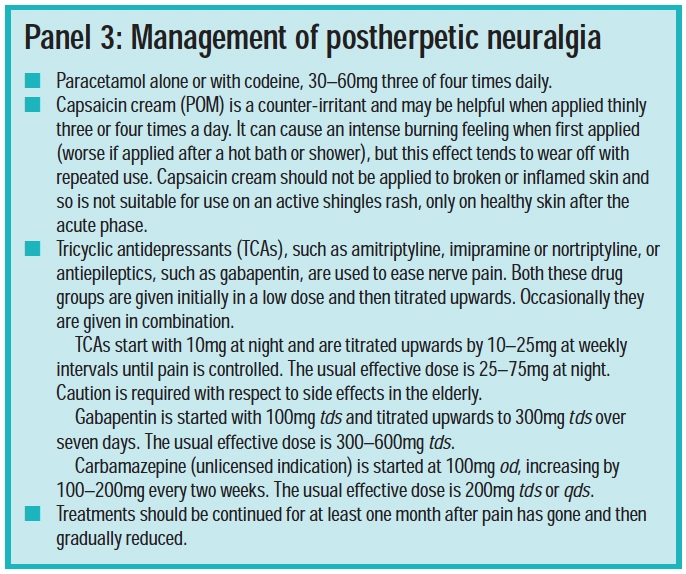
Postherpetic neuralgia can continue for weeks (and sometimes years) after the rash has subsided and can cause significant distress. It is more likely following a severe shingles rash and in people over 50 years: 7 per cent of people aged 50–59 years compared with 34 per cent of people >80 years are affected. Postherpetic neuralgia is usually self-limiting. Panel 3 describes management of this condition.
Ocular damage
Ophthalmic zoster affecting the ophthalmic division of the trigeminal nerve results in ocular damage in 50 per cent of patients. The shingles rash appears on thefore head, nose and around the eye and all patients suspected of ophthalmic zoster should be seen by an ophthalmologist and be given antiviral medication within 72 hours of rashonset. Complications include conjunctivitis,scleritis, ocular motor palsies, epithelial keratitis, anterior uveitis and acute retinal necrosis. There is a greater incidence of postherpeticneuralgia (and this lasts longer) in people with ophthalmic zoster.
Muscle weakness
Motor zoster, leading toweakness of the muscles supplied by thenerve, is more likely at older ages and occursin 5–10 per cent of people. It is more common after cervical or lumbosacral zoster. Theprognosis is generally good.
Other complications of shingles include:
- Bacterial skin infection
- Scarring or altered pigmentation at the rash site
- Involvement of the external ear, with occasional damage to the middle and inner ears, resulting in deafness and vertigo
- Ramsay–Hunt syndrome (a rare unilateral facial palsy associated with pain and herpetic blisters in the external ear due to involvement of the geniculate ganglion of the facial nerve; full recovery only occurs in about 20 per cent of untreated cases)
- Autonomic zoster
- Encephalitis
Resources
- Prodigy guidance on chickenpox. Available at: www.prodigy.nhs.uk (accessed 18 May 2006).
- Prodigy guidance on shingles and postherpetic neuralgia. Available at: www.prodigy.nhs.uk (accessed 18 May 2006).
References
- www.eurosurveillance.org/em/v10n01/1001-222asp.
- Swingler G. Chickenpox. Clinical evidence. Available at: www.clinicalevidence.com (accessed 18 May 2006).
- Royal College of Obstetricians and Gynaecologists. Chickenpox in pregnancy. Available at: www.rcog.org.uk (accessed 18 May 2006).
- Skorin L. Herpes zoster opthalmicus. Available at: www.optometry.co.uk (accessed 18 May 2006).
- Oxman MN, Levin MJ, Johnson GR, Schmader KE, Straus SE, Gelb, LD et al. A vaccine to prevent herpes zoster and postherpetic neuralgia in older adults. Available at: http://content.nejm.org (accessed 18 May 2006).
Action: practice points
Reading is only one way to undertake CPD and the Society will expect to see various approaches in a pharmacist’s CPD portfolio.
- Train your staff on what products to recommend for itching caused by chickenpox and why. What are the contraindications?
- Revise the indications and side effects of aciclovir, famciclovir and valaciclovir.
- Do you think children in the UK should be immunised against chickenpox? Discuss with another healthcare professional.
Evaluate
For your work to be presented as CPD, you need to evaluate your reading and any other activities. Answer the following questions: What have you learnt? How has it added value to your practice? (Have you applied this learning or had any feedback?) What will you do now and how will this be achieved?
You might also be interested in…

Norovirus and strategies for infection control

Case-based learning: insect bites and stings
