UC San Diego School of Medicine
Tamoxifen, used for prevention and treatment of breast cancer, has been shown to enhance the antibacterial activity of white blood cells in a study published in Nature Communications
[1]
on 13 October 2015.
Researchers at the University of California San Diego (UCSD) also found that tamoxifen treatment in mice enhances clearance of meticillin-resistant Staphylococcus aureus (MRSA).
Multidrug-resistant bacterial pathogens are on the rise, and the antibiotics pipeline is drying up, according to senior author Victor Nizet, professor of paediatrics and pharmacy. “We need to open the medicine cabinet and take a closer look at the potential infection-fighting properties of other drugs that we already know are safe for patients,” he says. In this way, Nizet’s team have discovered that tamoxifen has pharmacological properties that could aid the immune system in cases where a patient is immunocompromised or where traditional antibiotics have otherwise failed.
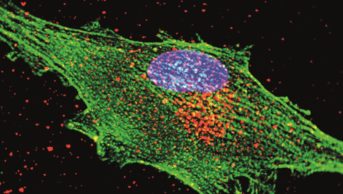
Tamoxifen targets the oestrogen receptor that is prevalent in hormone receptor-positive breast cancer. But the drug also affects the way that cells produce fatty molecules called sphingolipids. One type of sphingolipid, called ceramide, regulates the activity of a group of bacteria-killing immune cells called neutrophils.
“Tamoxifen’s effect on ceramides led us to wonder if, when it is administered in patients, the drug would also affect neutrophil behaviour,” says first author Ross Corriden, project scientist at the UCSD School of Medicine.
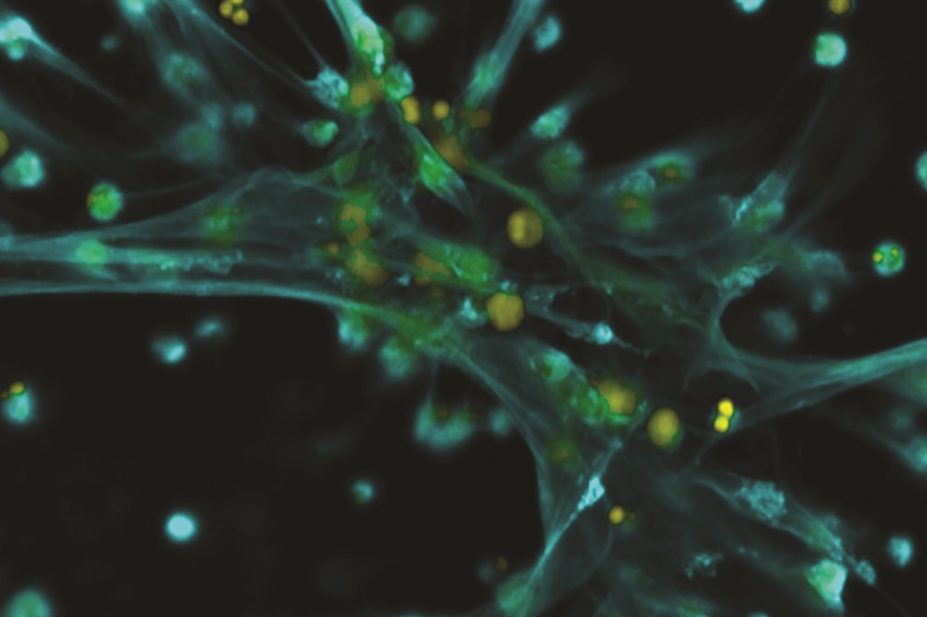
The researchers treated neutrophils with tamoxifen, and found that the cells were better at migrating towards and engulfing bacteria. The treated neutrophils also produced significantly more so-called neutrophil extracellular traps (NETs), a mesh of DNA, antimicrobial peptides, enzymes and other proteins that trap and kill bacteria. Similarly, the team showed that treating mice with tamoxifen increased their resilience against MRSA infection.
“While known for its efficacy against breast cancer cells, many other cell types are also exposed to Tamoxifen. The ‘off-target effects’ we identified in this study could have critical clinical implications given the large number of patients who take tamoxifen, often every day for years,” says Nizet.
Nizet and his colleagues from UCSD have previously shown a similar off-target effect for statins, which also enhance the formation of the extracellular traps formed by neutrophils[2]
.
It remains unclear whether the concentration of either of these drugs as they are currently used (to treat breast cancer or lower cholesterol) will retain these antibacterial properties. “At some of the higher concentrations reached in the body, these drugs may affect neutrophil activity; we are currently investigating minimum doses needed to achieve such effects,” says Nizet. “It has been shown in retrospective clinical data that patients taking statins may have lower risk of severe bacterial infections – changes in neutrophil function could be one factor.”
The promise of repositioning approved drugs has attracted much attention, particularly in light of the increasingly urgent need for new antibiotics. Juan Carlos Palomino and Anandi Martin from Ghent University, Belgium, have looked at the repositioning of drugs as a viable alternative in the treatment of tuberculosis. “We should not shy away from looking for alternative treatment options among already approved drugs,” they argue, citing the example of a long-established antipsychotic, thioridazine, and its anti-Mycobacterium tuberculosis activity in vitro, ex vivo and in vivo
[3]
.
“Recommendations on the use of these repurposed drugs must follow strict criteria and careful administration to avoid the risk of a rapid development of drug resistance,” Palomino and Martin warn. “We all know that, in the end, it remains a constant combat between us and the pathogen.”
Nizet and his team believe a substantial number of additional drugs may have off-target effects that modulate neutrophil activity. “We are testing several other drugs, including some FDA approved compounds, in ongoing studies,” he says.
“We believe this is incredibly important,” says Nizet. “Repurposing drugs for which the safety profile has already been assessed will greatly accelerate the development of new anti-infective therapies.”
References
[1] Corriden R, Hollands A, Olson J et al. Tamoxifen augments the innate immune function of neutrophils through modulation of intracellular Ceramide. Nature Communications 2015. doi:10.1038/ncomms9369
[2] Chow OA, von Köckritz-Blickwede M, Bright AT et al. Statins enhance formation of phagocyte extracellular traps. Cell Host Microbe 2010;8(5):445–454. doi:10.1016/j.chom.2010.10.005
[3] Palomino JC & Martin A. Is repositioning of drugs a viable alternative in the treatment of tuberculosis? Journal of Antimicrobial Chemotherapy 2013;68(2):275–283. doi:10.1093/jac/dks405