
Mclean/Shutterstock.com
In the dead of winter, under the UK’s gloomy cloud cover, concerns over vitamin D deficiency are growing. Short days and long nights offer little chance for the skin to absorb sunlight — an essential ingredient for vitamin D production. As many as 20% of UK adults have insufficient vitamin D levels, and hospitalisation rates for children with rickets — a bone-deforming disease caused by a lack of vitamin D — are now the highest in five decades[1]
,[2]
.
As a result, many people are trying to top up their vitamin D levels with supplements and, in 2018, £103m worth of prescriptions for vitamin D were issued in England alone (see Figure)[3]
. Vitamin D supplements are touted for many reasons: for bone and muscle health, respiratory infections, cardiovascular disease, cancer, fatigue, and even to prevent schizophrenia.
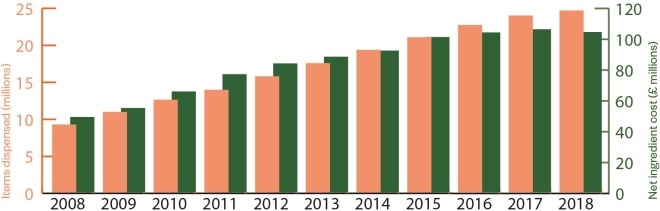
Figure: Increasing use of vitamin D
Source: Source: NHS Digital
In 2016, Public Health England (PHE) recommended that everyone should be taking supplements during the winter, and that those at higher risk of deficiency — such as infants, older people, and those in black, Asian and minority ethnic (BAME) groups — should be taking them year-round[1]
. However, a number of recent studies have challenged the enthusiasm for vitamin D supplements. A meta-analysis of 81 trials in 2018 found no benefit of taking vitamin D supplements for musculoskeletal health, and three large, randomised controlled trials in 2019 found no benefits for cardiovascular disease, cancer, diabetes or acute respiratory infections[4]
,[5]
,[6]
,[7]
.
Vitamin D is having a bit of a tough time at the moment with these big null randomised trials coming out
“Vitamin D is having a bit of a tough time at the moment with these big null randomised trials coming out,” says Adrian Martineau, an expert in respiratory infection and immunity at Queen Mary University of London, whose research has found some benefits of vitamin D supplements on acute respiratory illnesses and antibiotic-resistant tuberculosis
[8]
,[9]
.
Although no one disputes that vitamin D is an essential nutrient for human health, its benefits in capsule form may only go so far. Vitamin D supplements may not do much for those already getting enough of the vitamin through sunlight and diet, and they often are not taken by people who need them the most. Whether the null findings from the new trials, conducted outside of the UK, apply to the UK’s vitamin D-challenged population remains unclear, but vitamin D deficiency remains a priority for UK public health experts.
Raising vitamin D levels in other ways may help, such as “little and often” sunlight exposure, eating foods rich in vitamin D and food fortification.
Essentially there’s a kind of a disconnect between the aspiration, which is that everyone should receive 10 micrograms of vitamin D per day, and the reality, which is that that’s simply not happening
“Essentially there’s a kind of a disconnect between the aspiration, which is that everyone should receive 10 micrograms of vitamin D per day, and the reality, which is that that’s simply not happening,” Martineau says.
The sunshine vitamin
Vitamin D is a fat-soluble nutrient present in some foods, such as oily fish, egg yolks and red meat. Unlike other vitamins, vitamin D can also be synthesised by the skin from ultraviolet light and cholesterol. It is broken down by the liver and kidneys to produce an active form which aids absorption of calcium, magnesium, and phosphate.
The vitamin’s role in calcium absorption paved the way to its discovery: scientists first isolated it as a component of cod liver oil that cured rickets-like bone deformities in rats[10]
.
Observational studies have long drawn connections between vitamin D and health, but there is no consensus on how they should be interpreted; they could simply mean that unhealthy people are more likely to stay indoors. Study designs that introduce vitamin D supplementation are better at separating cause from consequence, and these have led to many suggestive links between vitamin D capsules and health.
With the literature awash with only slightly promising results, researchers have turned to meta-analyses and large trials to try to distinguish the true effects of vitamin D supplementation. However, so far, there have been no big signals, not even for musculoskeletal outcomes. In the recent 81-trial meta-analysis, no benefits were found, regardless of whether the researchers were analysing by dose, frequency of dosing, baseline levels of vitamin D, or the increase in vitamin D levels
[4].
“However we teased the evidence, we couldn’t convincingly find an effect for different subgroups,” says Alison Avenell, an expert in health services research at the University of Aberdeen and an author of the study.
Other trials involving thousands of people have come up empty-handed, too. The Vitamin D and omega-3 trial (VITAL), which involved more than 25,000 participants, found that taking vitamin D supplements daily for five years, at a dose of 2,000 international units (IU) or 50 micrograms per day, did not decrease the risk of cancer or cardiovascular events; whether there is a benefit for bone health has not yet been reported, though preliminary results suggest there is not[5]
,[11]
.
Another smaller study even found high doses (up to 10,000 IU) of vitamin D to be associated with adverse effects on bone density[12]
.
However, researchers are quick to point out that the negative results in these and other trials do not mean that vitamin D is useless. At the most, they show that vitamin D supplementation does not offer any benefit unless the person is “profoundly deficient” of vitamin D, Avenell suggests.
Definitions of vitamin D insufficiency vary. In the UK, anyone with a blood level of less than 25 nanomol/L of 25-hydroxyvitamin D (25(OH)D), a vitamin D metabolite, is deemed deficient. Other countries define insufficiency as anything below 40 nanomol/L. It also remains unclear how long a person must be below a given threshold before they start experiencing adverse effects.
The NHS is prescribing it at great cost, without evidence that it’s actually doing anything to prevent fractures and falls
However, in terms of identifying effective interventions for bone health, there is sufficient evidence to conclude that vitamin D supplementation is not one of them, Avenell says. “The NHS [is] prescribing it at great cost, without evidence that it’s actually doing anything to prevent fractures and falls,” she says.
Population protection
Nevertheless, it is possible that the UK represents a different test case.
“I think there’s a big difference between UK and US populations in terms of baseline status,” Martineau says.
A couple of the large trials were conducted in the United States, which is mostly south of the UK, leading to increased exposure to winter sunlight. The United States also has a tendency to fortify more food with vitamin D — such as milk — compared with the UK. As a result, only 7% of the US population is estimated to have a 25(OH)D level below 30 nanomol/L[13]
.
Low vitamin D status is particularly pronounced in BAME groups, owing to the fact that darker skin produces far less vitamin D than lighter skin per unit of ultraviolet light exposure[14]
. This is particularly problematic in countries with low levels of winter sunlight, like the UK. One study found that 79% of South Asian women in southern England had 25(OH)D levels below 25 nanomol/L in the autumn, compared with 4% of white women[15]
.
This problem is made all the more apparent when the seemingly rare rickets incidence rate of 8 in 100,000 white children rises to 95 in 100,000 BAME children[14]
.
In 2018, researchers in Birmingham, West Midlands, identified three babies with vitamin D deficiency-related cardiac arrest, seizures and rickets; one of whom died[16]
. These tragic cases highlight a need to intensify education about the risks of vitamin D deficiency particularly in babies, pregnant women and BAME groups[14]
.
With rising awareness of low vitamin D levels in the UK, PHE convened a Scientific Advisory Committee on Nutrition (SACN) for vitamin D to examine the evidence and set a dietary requirement in a report published in 2016[1]
. Before the report, it was thought that people could get all the vitamin D they needed from the sun. However, after establishing that musculoskeletal health was at risk when 25(OH)D levels dropped below 25 nanomol/L, the committee determined that a person would need to consume 10 micrograms of vitamin D per day to reach 25 nanomol/L, assuming the absence of sunlight-derived vitamin D. Remarkably, the average UK adult only obtains 2–3 micrograms per day from their diet.
Certainly, going from no recommendation for a dietary source to a recommendation was a big jump
“Certainly, going from no recommendation for a dietary source to a recommendation was a big jump,” says Hilary Powers, a retired professor of nutritional biochemistry at the University of Sheffield, who chaired the SACN on vitamin D.
By not taking into account any sunlight-derived vitamin D, the dietary requirement is, effectively, a worst-case scenario. But it captures the needs of almost everyone in the UK, including BAME populations, those who wear body-covering garments, pregnant women and infants, and those who do not go outside very often.
Supplementing vitamin D
PHE turned this dietary requirement into actionable advice in its 2016 guidance: those in at-risk groups should take vitamin D supplements year-round, whereas everyone else “should consider” vitamin D supplementation in autumn and winter[17]
.
The guidance cannot be more explicit because of difficulties in identifying those with low vitamin D status, since it is not necessarily accompanied by outward symptoms of deficiency and it requires a blood test to measure.
Testing has increased in the UK, with the combined costs of vitamin D tests and prescriptions increasing from £1,647 per 100,000 person-years in 2008 to £28,913 per 100,000 person-years in 2014, although it is important to note that the commonly used immunoassay is prone to false positive findings of deficiency[18]
[19]
.
PHE is not compelled to change its guidance in light of the new trials, mainly because it is not about musculoskeletal health, says Louis Levy, head of nutrition science at the agency. The meta-analysis does not persuade PHE either, because it is one study which lacks analysis of studies of individuals with poor vitamin D status — the focus of the PHE recommendation. The issue may be revisited in the future, however, Levy adds.
SACN undertakes regular horizon scanning and may consider this issue again in the future if it is of the view that the evidence base has substantially changed
“SACN undertakes regular horizon scanning and may consider this issue again in the future if it is of the view that the evidence base has substantially changed,” he notes.
In the meantime, the government provides free supplements for some people on low incomes; however, it is likely that these supplements do not reach everyone who needs them.
“People who tend to take nutrient supplements are those who least need them. In this country, it would be those who are white, middle class, very active, don’t smoke, and have a great diet,” Powers says, adding that there have been “many” studies that show this[20]
.
“So, there are problems in terms of a public health message that relies on supplements,” she adds.
Reminding people about sunlight as a vitamin D source could help boost levels, although fear of skin cancer and the resultant use of sunscreen complicates this. A research group at the University of Manchester recently espoused a “little and often” approach for sunlight exposure, without sunscreen, to garner enough vitamin D without increasing cancer risk. For people with fair skin, they recommended daily exposure for 10–15 minutes in the spring and summer to avoid vitamin D deficiency year round, whereas 25–40 minute exposures for BAME individuals would help them during the summer only[21]
.
Another approach is to add vitamin D to common foods. A recent study explored the fortification of flour and found it to be a cost-effective way to reduce cases of vitamin D deficiency by 25% in England and Wales[22]
.
“Bio-fortification” aims to produce foods with higher nutritional value. For example, chicken feed enriched with vitamin D increases the resulting eggs’ vitamin D levels, as well as consumers’ levels[23]
. Exposing mushrooms to ultraviolet radiation can also turn them into vitamin D-rich sources[24]
.
The experiences of other countries, such as the United States, Sweden, and Finland, show that fortification is more effective than supplement-taking, Martineau says.
“It’s much more effective at boosting population status because people don’t have to do anything about it,” he continues.
“If we could achieve [the recommended intake via fortification], it would be a major public health victory.”
References
[1] Public Health England. 2016. Available at: https://www.gov.uk/government/publications/sacn-vitamin-d-and-health-report (accessed January 2020)
[2] Goldacre M, Hall N & Yeates DG. Lancet 2014;383(9917):597–598. doi: 10.1016/S0140-6736(14)60211-7
[3] NHS Digital. 2019. Available at: https://digital.nhs.uk/data-and-information/publications/statistical/prescription-cost-analysis/2018 (accessed January 2020)
[4] Bolland MJ, Grey A & Avenell A. Lancet Diabetes Endocrinol 2018;6(11):847–858. doi: 10.1016/S2213-8587(18)30265-1
[5] Manson JE, Cook NR, Lee IM et al. N Engl J Med 2019;380(1):33–44. doi: 0.1056/NEJMoa1809944
[6] Pittas AG, Dawson-Hughes, Sheehan P et al. N Engl J Med 2019;381(6):520–530. doi: 0.1056/NEJMoa1900906
Pittas AG, Dawson-Hughes, Sheehan P et al. N Engl J Med. 2019;381(6):520–530. doi: 10.1056/NEJMoa1900906
[7] Camargo CA, Sluyter J, Stewart AW et al. Clin Infec Dis 2019; In press. doi: 10.1093/cid/ciz801
[8] Martineau AR, Joliffe DA, Hooper RL et al. BMJ 2017;356:i6583. doi: 10.1136/bmj.i6583
[9] Jolliffe DA, Ganmaa D, Wejse C et al. Eur Respir J 2019;53(3). doi: 10.1183/13993003.02003-2018
[10] Rajakumar K. Pediatrics 2003;112(2):e132–135. doi: 10.1542/peds.112.2.e132
[11] Hlavinka E. 2019. Available at: https://www.medpagetoday.com/meetingcoverage/asbmr/82341 (accessed January 2020)
[12] Burt LA, Billington EO, Rose MS et al. JAMA 2019;322(8):736–745. doi: 10.1001/jama.2019.11889
[13] Schleicher RL, Sternberg MR, Lacher DA et al. Am J Clin Nutr 2016;104(2):454–461. doi: 10.3945/ajcn.115.127985
[14] Uday S & Högler W. Arch Dis Child 2018;103(9):901–906. doi: 10.1136/archdischild-2018-314826
[15] Darling AL, Hart KH, Macdonald HM et al. Osteoporos Int 2013;24(2):477–488. doi: 10.1007/s00198-012-1973-2
[16] Uday S, Fratzl-Zelman N, Roschger P et al. BMC Paediatr 2018;18 (1):183. doi: 10.1186/s12887-018-1159-y.
[17] Public Health England. 2019. Available at: https://www.gov.uk/government/news/phe-publishes-new-advice-on-vitamin-d (accessed January 2020)
[18] Basatemur E, Hunter R, Horsfall L et al. Eur J Pediatr 2017;176(10):1405–1409. doi: 10.1007/s00431-017-2986-9
[19] Avenell A, Bolland MJ, Grey A et al. Ann Clin Biochem 2018;56(2):188–189. doi: 10.1177/0004563218796858
[20] Kofoed CL, Christensen J, Dragsted LO et al. Brit J Nutr 2015;28;113(12):1993–2000. doi: 10.1017/S0007114515001440
[21] Burchell K, Webb A & Rhodes L. 2019. Available at: https://www.research.manchester.ac.uk/portal/en/publications/sunlight-exposure-and-vitamin-d(22b3e7e8-9327-4087-9466-d3f1ed8736ad).html (Accessed January 2020)
[22] Aguiar M, Andronis L, Pallan M et al. Eur J Clin Nutr 2019; In press. doi: 10.1038/s41430-019-0486-x
[23] Hayes A, Duffy S, O’Grady M et al. Am J Clin Nutr 2016;104(3):629–637. doi: 10.3945/acjn.116.132530
[24] Cashman KD, Kiely M, Seamans KM & Urbain P. J Nutr 2016;146(3):565–575. doi: 10.3945/jn.115.223784

