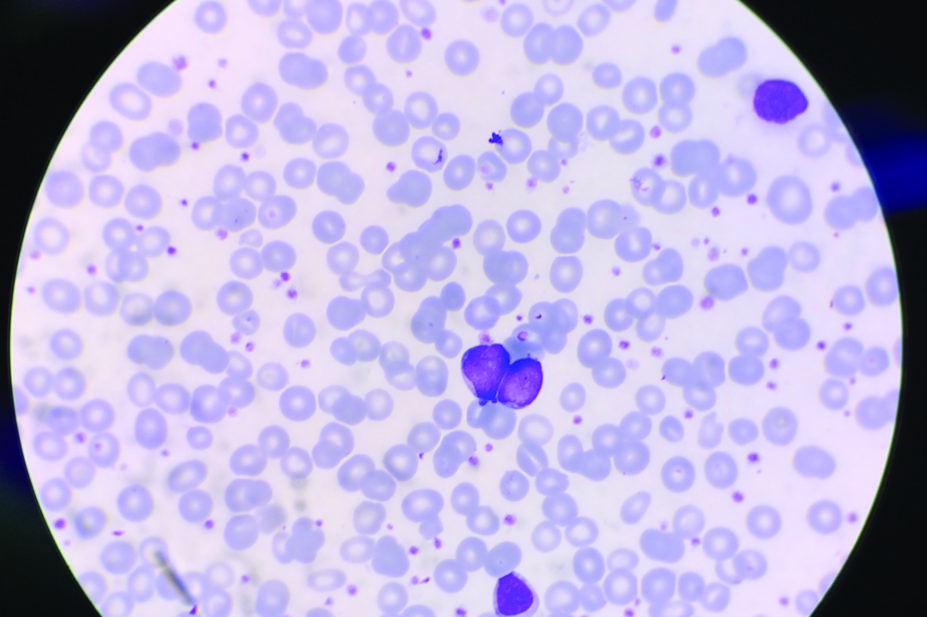
Shutterstock.com
A raised platelet count or thrombocytosis is a risk indicator of cancer in adults, according to the results of the first large-scale study of its kind published in the British Journal of General Practice
[1]
(online, 22 May 2017).
Researchers found that thrombocytosis was found in 11.6% of men and 6.2% in women who developed cancer – the figures are high enough to warrant a GP referral for suspected cancer according to existing guidance from National Institute for Health and Care Excellence (NICE), England’s health technology assessment body.
The researchers say: “These figures are well above the 3% threshold used by NICE for suspected cancer investigation, and strongly suggest that cancer should be considered in patients showing thrombocytosis.”
They based their findings on statistics from the UK Clinical Practice Research Datalink, which holds anonymised electronic primary care records from roughly eight per cent of UK practices.
They compared the incidence of cancer in a 12-month period between two groups of patients — 31,261 aged under 40 who had thrombocytosis and another group of 7,969 matched patients who had a normal platelet count.
They found that 1,098 out of 9,435 males with thrombocytosis were diagnosed with cancer within the time frame (11.6%; 95% confidence interval [CI] = 11.0 to 12.3), compared with 106 of 2,599 males without thrombocytosis (4.1%; 95% CI = 3.4 to 4.9).
When they focused on female patients they found 1,355 out of a total of 21,826 with thrombocytosis developed cancer (6.2%; 95% CI = 5.9 to 6.5), compared with 119 of 5,370 females without a high platelet count (2.2%; 95% CI = 1.8 to 2.6).
The cancer risk increased to 18.1% (95% CI = 15.9 to 20.5) for males and 10.1% (95% CI = 9.0 to 11.3) for females, when a second raised platelet count was recorded within six months.
The incidence of cancer rose with age and with a higher platelet count; at least a third of patients with lung and colorectal cancer who had pre-diagnosis thrombocytosis had no other symptoms which would indicate malignancy.
They say: “This analysis shows that only two-thirds of patients had symptoms that would be recommended for urgent investigation in current NICE guidance; one-third had no relevant symptoms in the year before diagnosis, other than thrombocytosis.
“It is in this group that thrombocytosis has the greatest potential to prompt earlier diagnosis, where other symptoms have not yet developed. This strongly suggests that cancer should be considered when a result is received showing thrombocytosis, even if cancer was not initially suspected.”
The results of the study were welcomed by the charity Cancer Research UK.
Its health information officer Dr Jasmine Just, says: “There are lots of possible reasons why a person’s platelet count might be high, and in most cases it won’t be down to cancer.
“Measuring platelet count in patients who don’t otherwise warrant a blood test is not necessarily a good idea. But if a patient has a blood test for another reason and a high platelet count is found, then one of the possible diagnoses doctors should consider is cancer.
“More research is needed to confirm whether investigating people for cancer just based on a high platelet count would save lives.”
Helen Stokes-Lampard, chair of the Royal College of GPs says the findings are “interesting” and add to existing data known about high platelet counts.
She says GPs include platelet levels as part of the full blood count test which is routinely carried out in their surgeries.
References
[1] Bailey SE, Ukoumunne OC, Shephard EA et al. Clinical relevance of thrombocytosis in primary care: a prospective cohort study of cancer incidence using English electronic medical records and cancer registry data. Br J Gen Pract online, 22 May 2017. doi: 10.3399/bjgp17X691109
You may also be interested in

No clear evidence that cannabis-based medicines are successful treatment for chronic pain

Almost 90% of pharmacies report abuse from ineligible COVID-19 vaccination patients, survey reveals
