Shutterstock.com
With just over 14 months to go until the Falsified Medicines Directive (FMD) is fully incorporated into UK law, a Pharmaceutical Journal survey has revealed that the majority of pharmacists, while supporting FMD in principle, remain concerned about how the law will operate in practice.
FMD is an EU-wide legislation which aims to provide a secure supply chain from manufacturers through wholesale and pre-wholesale to dispensers and, finally, patients. It is due to go live on 9 February 2019.
The Medicines and Healthcare products Regulatory Agency (MHRA) has UK-wide responsibility for working out how best to put FMD into UK law and is working on the matter through the FMD Implementation Advisory Board.
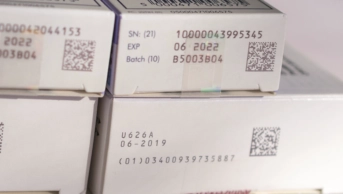
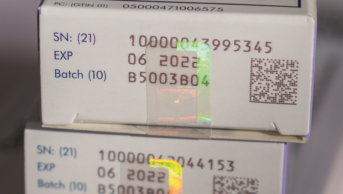
Once made law, medicine packs will have to be issued with a tamper-proof security seal and a unique identifier. The latter, embedded in a 2D barcode, will allow the medicine to be tracked through the supply chain from manufacturer to patient. Each pack’s unique identification data will be stored in an EU-wide central hub called the European Medicines Verification System (EMVS).
UK pharmacies, wholesalers and manufacturers will connect to the EMVS though the UK Medicines Verification System (UK MVS), which is currently being developed by SecurMed UK and Arvato Systems.
Once FMD goes live in the UK, a medicine pack’s barcode must be scanned by a pharmacist and recognised by the EMVS as authentic. A pilot of the UK MVS is scheduled to begin in early 2018.
However, the PJ’s survey of 656 Royal Pharmaceutical Society members revealed that more than a quarter (27%) were unaware of the date that FMD is due to be fully incorporated into UK law. Of the 73% who were aware, nearly three-quarters (72%) said they did not fully understand how FMD would affect their work.
According to the survey, which was sent out in August 2017, 71% of 481 respondents said they were concerned about increased workload as a result of FMD. This concern was expressed by 79% of community pharmacists and 75% of hospital pharmacists, but only 50% of pharmacists based in industry.
Some 58% of respondents said they were worried about the cost of becoming FMD-compliant. Again, there was variation across the sector: 61% of community pharmacists and 66% of hospital pharmacists expressed concern, compared with 44% of industry-based pharmacists. Scottish pharmacists were less worried than those working elsewhere in Great Britain, according to the survey, with 45% saying that they were concerned compared with 64% of English and 60% of Welsh pharmacists.
Out of all respondents (481), 52% said that they were worried about the impact FMD procedures would have on patient services. This worry was more pronounced among community and hospital pharmacists — 58% and 56%, respectively — but only shared by 34% of those working in industry.
Community pharmacists expressed specific concerns that patients might have to wait longer for their prescriptions, and questioned how the law would operate with monitored dosage system (MDS) and compliance trays. The question of split packs, too, was raised by several community pharmacists, who were concerned that scanning a previously-split pack for a second time would flag up that pack as counterfeit. However, others were more optimistic, and felt that, as with any new process, initial challenges would soon “settle down”. Again, Scotland expressed less concern than the other two GB nations: 45%, compared with 56% in England and 68% in Wales.
Jerome Bertin, managing director of SecurMed — the not-for-profit organisation tasked with delivering the UK’s medicines verification system — said that the survey results demonstrated that “the message is still getting out”.
He added that communications around FMD were being managed by the Medicines and Healthcare products Regulatory Agency (MHRA) and the Department of Health (DH), with further information being provided by the UK FMD Working Group for Community Pharmacy.
Responding to specific concerns over increased workload, he said: “FMD is going to be a big change in terms of working practice. After the initial flux in the system, it’s going to take several years for non-FMD compliant packs to exit the supply chain, so there will be a long changeover period. There will be false positives and negatives flagged up by the IT system during this initial flux, but that will improve in time. Cost is a key issue, as each stakeholder group is responsible for implementing FMD systems. Hospital and community pharmacy sectors need to take this up with negotiating bodies.”
A clear majority of survey respondents supported the introduction of FMD with 68% of 546 GB pharmacists believing FMD to be necessary. Industrial and hospital pharmacists were in close agreement: 84% and 80% respectively compared with 61% of community pharmacists.
Pharmacists working in Scotland and Wales were slightly more convinced of the need for FMD than their colleagues in England, with 82% of pharmacists in Scotland and 80% of pharmacists in Wales saying the law was necessary, compared with 63% respondents based in England.
Those who did not feel FMD was necessary cited the existing security of the UK medicines supply chain, and the fact that very few counterfeit medicines have found their way into registered UK pharmacies. Other respondents said that while they felt FMD was necessary, the law should be more focused on high-value medicines, which are more likely to be subject to counterfeiting, rather than on generic and low-cost drugs.
In support of FMD, one respondent pointed out that while legally responsible for the quality of the medicines they supply, pharmacists currently have no way — beyond visually assessing packaging quality — to verify the authenticity of medicines on their shelves. Others felt that opting out of FMD post-Brexit would leave the UK at a disadvantage — a “weak link” — in the global supply chain. To ignore the possibility of counterfeiting, said one respondent, would be a failure to demonstrate a pharmacist’s duty of care.
The next meeting of the joint DH/MHRA FMD Implementation Advisory Board is scheduled for January 2018.
For further information on FMD and its implementation pharmacists are advised to visit www.securmed.org.uk, and the FMD Working Group for Community Pharmacy site.
Note on statistics
68 of the 656 survey respondents lived in countries outside of Great Britain. These respondents’ answers were not included in the overall statistics for the above four questions, but were included in the sector breakdowns of the responses to these questions
Falsified Medicines Directive
The Falsified Medicine’s Directive (FMD), which comes fully into force in February 2019, introduces EU-wide legislation to help prevent counterfeit prescription medicines entering the pharmaceutical supply chain. “Falsified” covers not only counterfeit medicines, but also false information about a medicine’s source. FMD will not cover non-prescribed medicines, with the single exception of omeprazole.
All medicines packs will be tamper-proof and will feature a 2-D barcode, as well as a manufacturer product code, a randomised unique serial number, batch number and expiry date.
Since 2011, the Royal Pharmaceutical Society and other stakeholders have been acting to ensure that the FMD will function in accordance with UK law, in a way that ensures patient safety, whilst minimising disruption to existing pharmacy practise.
The RPS has been acting on FMD since 2011, when it set up a multidisciplinary, cross-sectorial, GB-wide working group to develop policy. Later, in July 2014, the Society hosted and chaired the first FMD stakeholders networking meeting, at which 13 countries were represented by 100 delegates. At this meeting, implementation challenges for FMD were discussed, and presentations from the three main software providers were made.
Specific features of FMD in the UK lobbied for and achieved by the RPS and other stakeholders include:
- Extension of the originally-proposed two-day window for scanned products that are not collected by a patient to be returned to stock. This has been increased to ten days. Under FMD medicine not collected within the window will have to be destroyed, so extending the time limit reduces wastage.
- Agreement on the form of the European Stakeholder Model, which lays out a EU-wide format for how medicines can be verified, and on the European Medicines Verification System (EMVS), which guarantees authenticity from manufacturing to dispensing (the “end-to-end” system)
- Inclusion of human readable data alongside the 2-D barcode, so that pharmacists can continue to help patients if scanners break down or if the barcode is damaged.
- Full repackaging of imported medicines, rather than addition of new barcodes to existing packaging. Multiple barcodes could result in incorrect barcodes being scanned, triggering a false exceptional event.
- Greater flexibility offered to hospitals on the timing of medicines decommissioning. FMD requires medicines to be decommissioned at the point of dispensing. In hospitals – particularly in A&E, and where single doses are administered – this isn’t practical. Following lobbying, hospitals (unlike community pharmacies) will be able to decommission upon delivery, and then store medicines.
- Use of a single workstation. FMD originally required two, one for decommissioning and one for dispensing. RPS argued that this was unnecessary, costly, and increased the chance of technical failures disrupting processes. Successful lobbying led to agreement that all tasks can be performed on the Patient Medical Record (PMR) computer.
In addition, the RPS continues to call for the addition of safety information (including batch code, expiry dates and potential interactions) into the 2D barcode, alongside authentication data.