Abstract
Aim
To establish the national position with regard to the incorporation of electronic transfer/discharge and electronic prescribing into clinical settings, particularly chemotherapy.
Design, subjects and setting
Questionnaire.
Subjects and setting
Cancer network lead pharmacists across the UK.
Results
Overall response was 63%. Results showed that there were electronic chemotherapy prescribing systems in 32 per cent of trusts that responded and the availability of general electronic prescribing in 8 per cent. Nationally, there was significant variability in the systems available and in their compatibility with other systems.
Conclusion
The need for electronic systems is urgent. Unless the approach to this is well synchronised there is a real threat that that the NHS will never develop high-quality hospital-based electronic systems.
Electronic prescribing was introduced into GP practices in the early 1990s in an attempt to improve accuracy and efficiency and should now be fully operational. Similar progress has not been made in hospital practice.
The Connecting for Health (previously National Programme for Information Technology) e-prescribing programme aims to improve patient safety by facilitating the development and delivery of electronic prescribing systems. Connecting for Health recently stated that implementation will be challenging and will require acceptance of new ways of working.1
Working with the National Patient Safety Agency, Connecting for Health published guidelines recently on design-related safety features to be incorporated into electronic systems.2 This follows studies in hospitals in the UK where electronic prescribing systems are in place. Nationally, there is a range of systems, not all of which are compatible with each other.
A study in 2007, investigated the effectiveness of electronic prescribing in two UK hospitals. It found that electronic prescribing led to an overall reduction in prescribing errors in both hospitals. However, new types of error were identified at both sites, including inaccurate selection of drugs, drug doses and drug frequency from drop-down boxes and choosing incorrect default doses.3,4
The European Commission’s policy “i2010” aims to provide safe, efficient and good quality healthcare for all European citizens. The e-health action plan aims to stimulate investment and deployment of e-health solutions across Europe.5
In the US, the Medicare Improvements for Patients and Providers Act of 2008 offers financial incentives for doctors who use e-prescribing and penalties for those who do not. In 2007 of the four billion prescriptions written in the US, only 25 million were transmitted electronically. The main barrier to electronic prescribing is thought to be the cost of equipment, training and software.6
One specialty where there is a compelling need for electronic prescribing and documentation is cancer chemotherapy services. According to independent think tank Reform, much chemotherapy prescribing is paper-based and prone to error.7 One of the key recommendations on quality and safety from the National Chemotherapy Advisory Group relates to information technology. It states:“Electronic prescribing has been shown to promote patient safety by reducing errors. It also facilitates collection of standardised data. Those chemotherapy services that do not currently use electronic prescribing should strongly consider doing so.”8
In our view implementation of electronic processes in the field of oncology could provide useful information for other specialties. We have therefore surveyed cancer networks across the UK to establish whether systems were in place and operational for the use of electronic prescribing and electronic transfer/discharge summaries.We aimed to establish the position nationwide in oncology, to gain insight into other specialties with regard to the incorporation of electronic transfer/discharge letters and electronic prescribing into their clinical settings and to explore the benefits and difficulties that may have been experienced with the systems used.
Our survey is a cancer-network facilitated review of the position of hospital-based electronic-prescribing systems in summer 2008: it is not current and there is no evidence to show that the systems are safe or robust. However, we believe that changes in the field of oncology could serve as a measure of change elsewhere and that the results of the survey could provide useful information for other areas of hospital medicine.
Methods
The survey was constructed in collaboration with an oncologist, a cytotoxics pharmacist and the hospital IT project manager. The British Oncology Pharmacy Association website was used to identify the UK cancer networks.
A covering letter was devised outlining the aims of the survey, which was then e-mailed to all cancer network pharmacists, who were asked to cascade it to pharmacy contacts in each trust in the network. This was to ensure the whole of the UK had been surveyed.
A deadline of one month was given for return of survey, followed by a one-month extension.A reminder e-mail to non-responders followed. At this point half the cancer networks had responded. One further reminder was e-mailed to the remaining non-responding networks, leading to an overall response rate of 63 per cent.
Results
A total of 24 out of the 38 cancer networks responded (63 per cent) and 38 trusts submitted completed surveys before the deadline (there were a number of trusts within each network) Responses were received from all four countries of the UK.
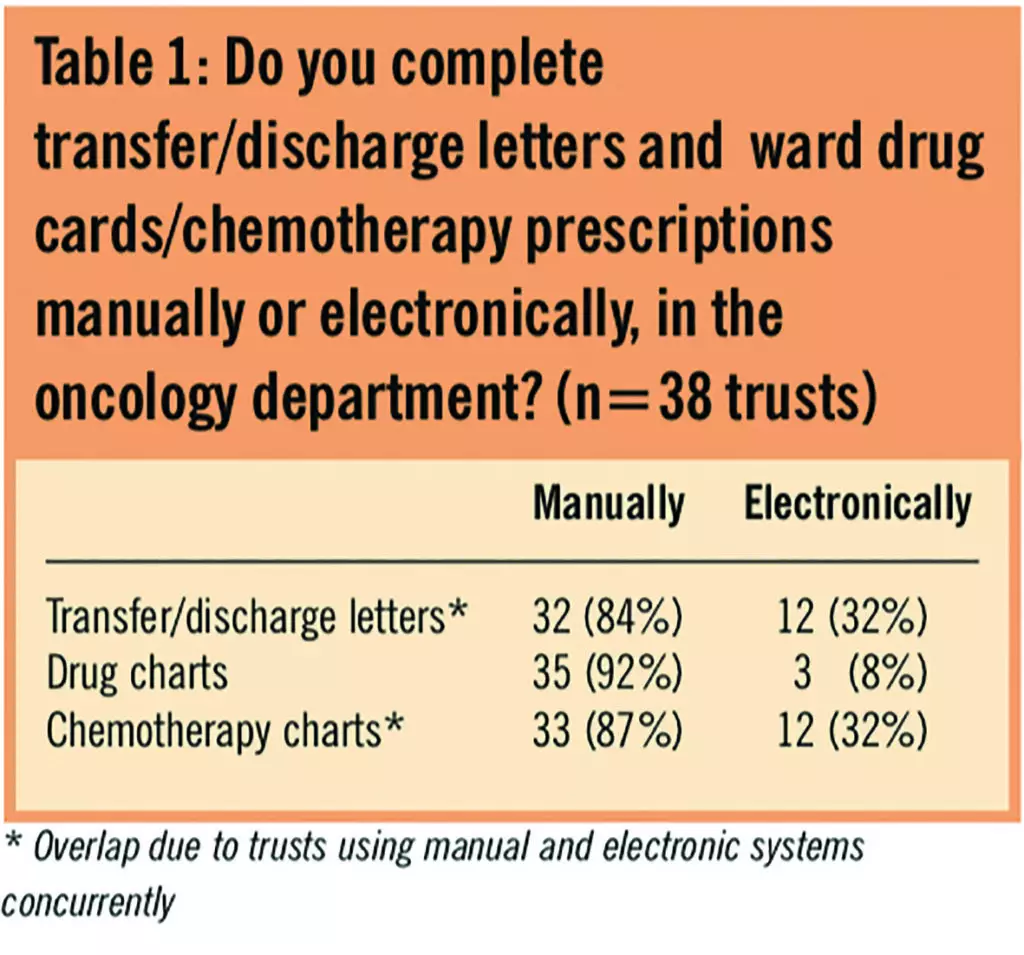
Where trusts had an electronic system in place, many appeared to use both manual and electronic types of system concurrently or when electronic systems failed (Table 1). Electronic chemotherapy prescribing systems were available in 32 per cent of trusts that responded and general electronic prescribing in 8 per cent (Table 1).
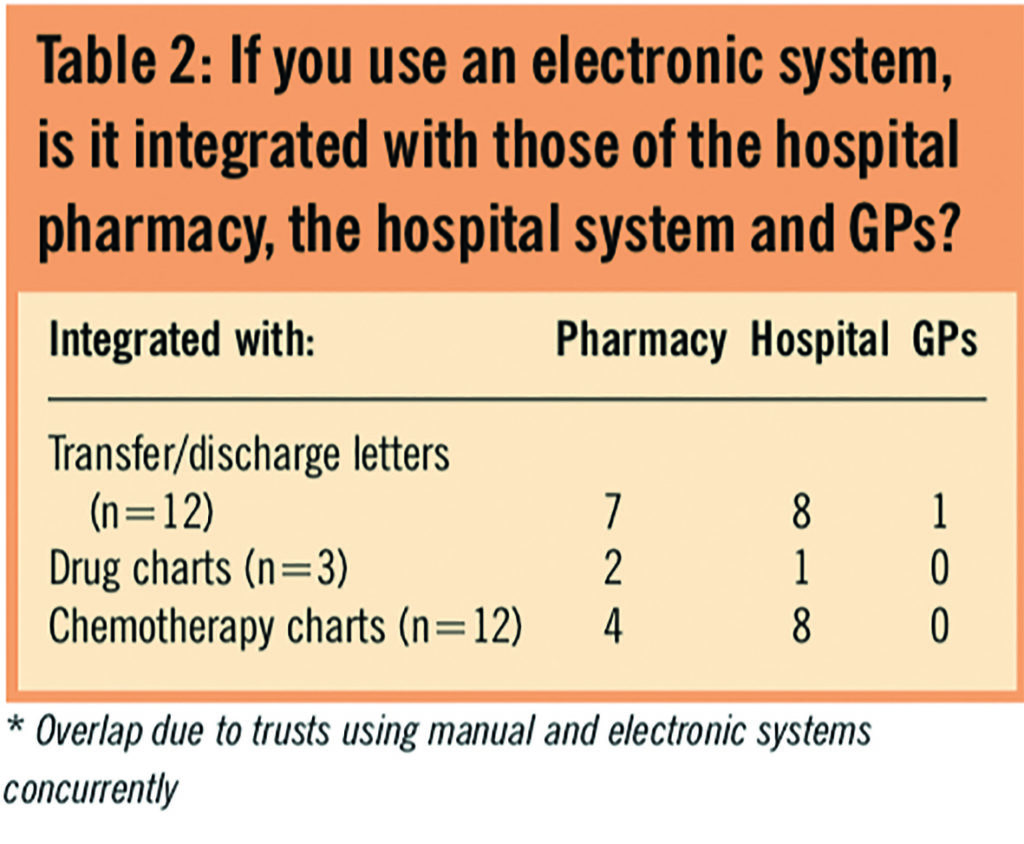
Of the trusts that had electronic systems, 30 per cent of electronic transfers/discharges were not integrated into pharmacy systems and 90 per cent were not linked to GP surgeries. The electronic prescribing used by one trust was integrated into the pharmacy and hospital systems (Table 2).
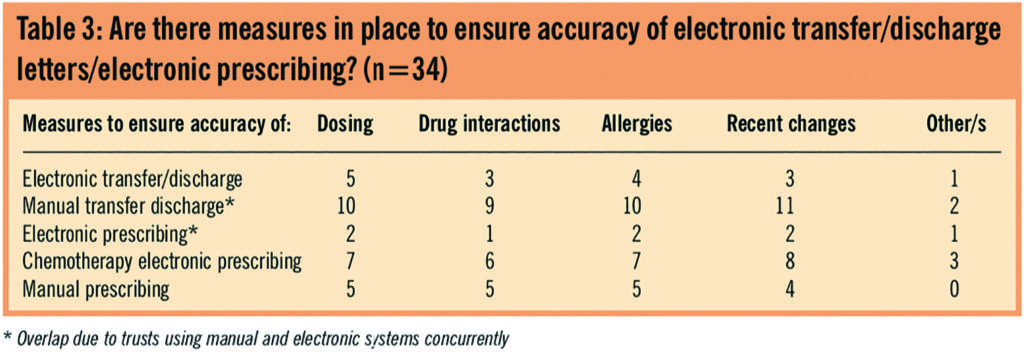
There were few responses to the question in Table 3. Many of the trusts using manual systems did not answer the question, although manual prescribing and manual transfers/discharges refer to handwritten versions and could have been answered by all trusts. Trusts using electronic prescribing had measures in place to ensure accuracy, as did most of the trusts using chemotherapy electronic prescribing. Most of the trusts using electronic transfer/discharge did not report having adequate measures in place to ensure accuracy.
When trusts were asked how many computers per patient they had on the wards on average trusts reported one computer for eight patients. However, in some trusts there were no computers on the wards.
When asked to name the systems used, respondents named 15 different systems. Many trusts used more than one system and had their own in-house electronic systems.
There were few responses when respondents were asked whether they were satisfied with their systems. The difference in satisfaction rates between electronic and manual systems seemed minimal.
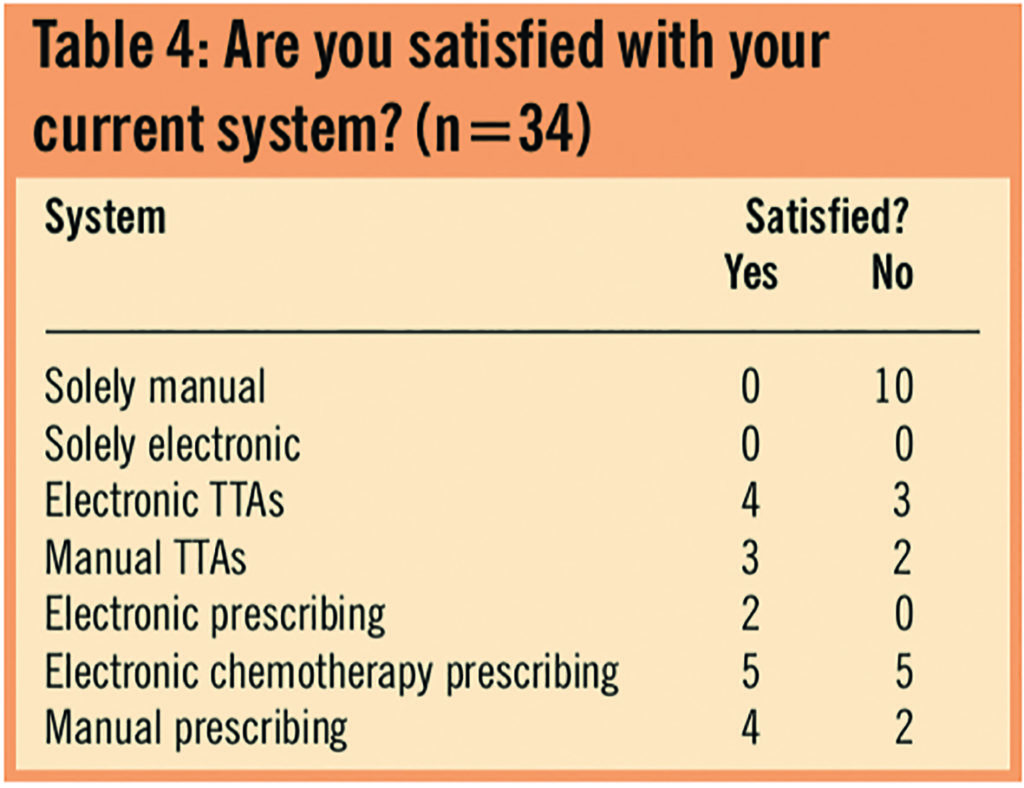
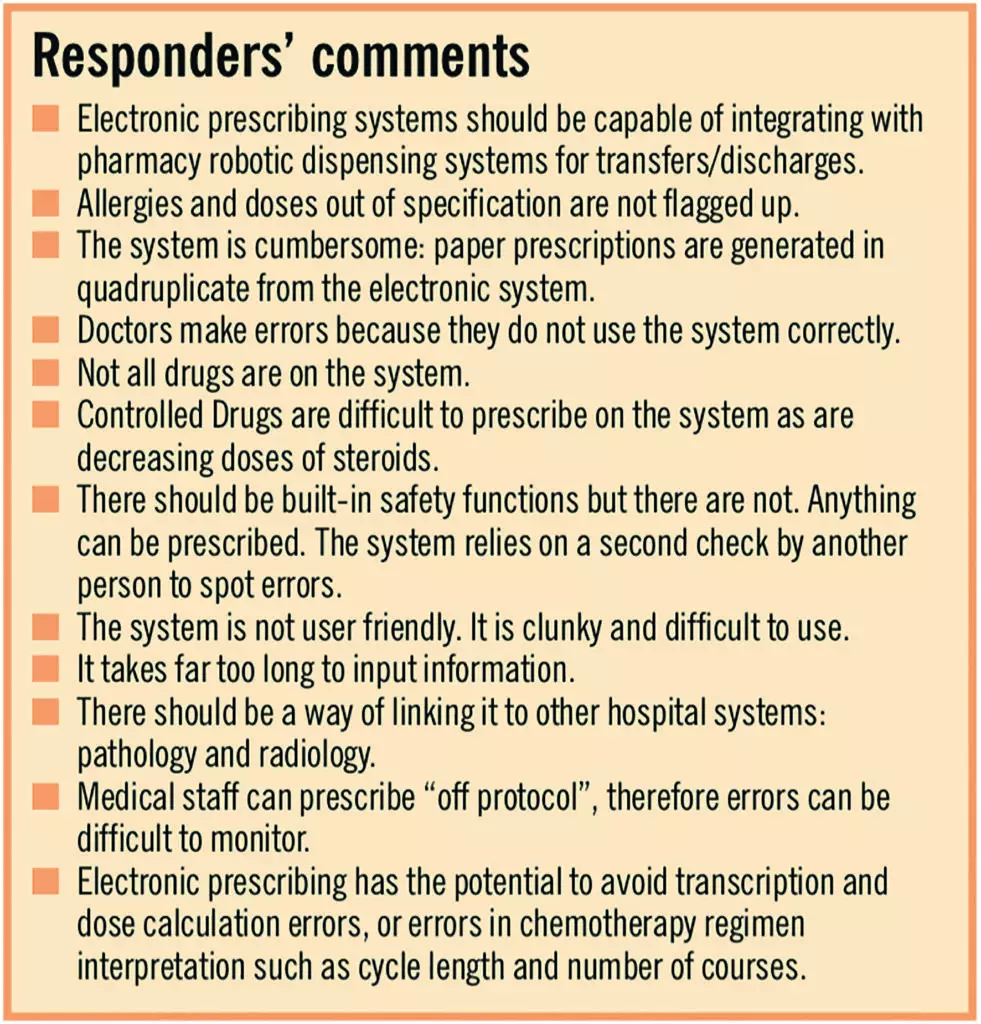
However, overall, from responders’ comments (see Panel), trusts do not seem to be entirely satisfied with electronic systems that are in place.
Discussion
The National Programme for Information Technology was created to modernise information technology across the NHS within a 10-year period, with an investment of £6.2 billion. In partnership with the National Patient Safety Agency, the NHS Connecting for Health’s overall aim is to promote safer working practices with the help of IT. In 2007, responsibility for delivery of the IT programme was transferred to strategic health authorities, all of which are working closely with NHS Connecting for Health to ease the transition.
According to independent think tank Reform, there is no coordinated national IT system in place to maximise the use of facilities across artificial administrative boundaries. Reform emphasised that most chemotherapy prescribing is paper-based, therefore prone to error that could have harmful or even fatal consequences. It recognised that the NpfIT did not have specific plans for electronic prescribing within oncology. Although many oncology-specific electronic prescribing programs are available, there is no national system to ensure these are adopted.8
- Nationwide electronic systems for transfer/discharge and electronic prescribing seem to be far from satisfactory
- Electronic systems are beginning to be introduced in trusts, but there is no co-ordinated approach, so the integration of different systems may be problematic
- There are issues of cost, staff training and lack of computers
- Responders appeared to be biased towards the negative aspects of systems used, whether manual or electronic
Although progress has been made locally, we have demonstrated in this survey a lack of uniformity with little, if any, national ownership of a national project. The need for electronic systems is compelling and even urgent. Unless the approach to this is well synchronised there is a real threat that the NHS will never develop high-quality hospital-based electronic systems.
Acknowledgements
We thank Ken Kennedy and Jane Mulreany, senior IT project manager, at Southend University Hospital NHS Foundation Trust for their input.
About the authors
Emma Traer, BSc, MBBS, is a specialist trainee year one doctor at Ipswich Hospital NHS Trust (previously foundation year two doctor at Southend University Hospital NHS Foundation Trust).
Krishnaswamy Madhavan, MBBS, FRCR, is consultant clinical oncologist at Southend University Hospital NHS Foundation Trust.
Correspondence to: Dr Madhavan (e-mail: krishnaswamy.madhavan@southend.nhs.uk)
References
- Connecting for Health electronic prescribing programme. Available at: www.connectingforhealth.nhs.uk/ (accessed 29 March 2010).
- Connecting for Health electronic prescribing programme. Available at: www.connectingforhealth.nhs.uk/ systemsandservices/electronicprescribingrescribing/ hazard_framework.pdf (accessed 29 March 2010).
- Donyai P, O’Grady K, Jacklin A, Barber N, Franklin BD. The effects of electronic prescribing on the quality of prescribing. British Journal of Clinical Pharmacology 2008;65:230–7.
- Barker A & Kay J. Electronic prescribing improves patient safety — an audit. Hospital Pharmacist 2007;14:225.
- eHealthNews EU Portal. ICT for Health i2010 — Transforming the European healthcare landscape. 19 June 2006. Available at: www.ehealtheurope.net/document_ library/policy_strategy_and_planning (accessed 5 May 2010).
- Sipkoff M. E-prescribing encouraged by new federal law. Drug Topics. 15 September 2008. Available at: http://drugtopics.modernmedicine.com (accessed 26 April 2010).
- Sikora K, Slevin M, Bosanquet N. Cancer Care in the NHS. London: Reform; 2005.
- NHS Cancer Action Team: Chemotherapy in England: ensuring quality and safety. A report from the National Cancer Advisory Group. 12 November 2008. Available at: www.dh.gov.uk (accessed 26 April 2010)
You may also be interested in

Reviewing prescribing practice in an adult critical care unit with a newly implemented electronic prescribing system
